I've been pretty absent from this space for a couple of months, and I think I know why. As a reporter, I'm more apt to write about my MDS when there's a story to tell. When it appeared that my Campath story had played itself out without a fully successful conclusion, I lost the plot line.
Yesterday, my MDS got its groove back.
I had a call from Dr. Bogdan Dumitriu, a fellow at the National Institutes of Health. I met Dr. Dumitriu during my follow-up visits in the Campath trial. He called today to share some very, very interesting news about my MDS.
When I signed up for the Campath trial at NIH, I also signed a separate protocol that allows the lab to take extra blood and bone marrow samples, for use in other research. One line of research being pursued by Dr. Neal Young, Dr. Phillip Scheinberg, and others involves telomeres.
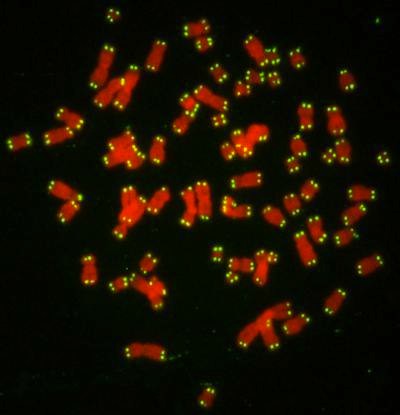
As I understand this, telomeres are little tails of material on the tip ends of chromosomes. They don't have much genetic significance, but they serve a very important protective function. When a chromosome divides, it's important that it splits at just the right place, so that a chunk of one of the new chromosomes doesn't get torn off and remain attached to the old chromosome. The telomere is where the split happens.
[IMG]
 071004143131-large
071004143131-large by
hankins.greg, on Flickr[/IMG]
The telomere is like a bit of sacrificial tissue at the break point that prevents the more important bits of the chromosome from being damaged during division.
As we get older, our telomeres get shorter, so they don't work as well to protect the important parts of the chromosome, and we're more likely to suffer chromosomal damage. It's possible that these shorter telomeres may be one of the causes of MDS -- and one of the reasons MDS is so much more common in older folks.
It turns out, Dr. Dumitriu tells me, that my telomeres were tested at NIH, and they are very, very short. What counts as "short" varies by age. As a 54-year-old, my telomeres are shorter than 99 percent of all other 54-year-olds. In other words, my age-adjusted telomere length places me in the first percentile of telomere shortness.
Every time a cell divides, it loses a bit of telomere. But some of that can be added back on by an enzyme called telomerase, which has a protein component called telomerase reverse transcriptase [TERT] and an RNA component called telomerase RNA component [TERC]. Both TERT and TERC have their respective genes, and, Dr. Dumitriu tells me, I have a mutated TERT.
There's not much telomerase in your garden variety human cell. It's only needed where there's a lot cell division going on. The bone marrow would be one place, since the marrow has to crank out billions of new blood cells every day. Another place would be in a tumor. Cancer cells divide so fast that they would literally work their little telomere tails off if they didn't have an ample dose of telomerase helping rebuild those tails.
Studies in the lab have shown that male sex hormones -- androgens -- can increase telomerase activity in bone marrow stem cells. Studies in people have shown that folks with TERT mutations and low telomerase activity can regain normal telomerase activity by taking androgens.
So, the NIH has developed a clinical trial using mail sex hormones -- in this case, a synthetic testosterone called Danazol -- in folks with aplastic anemia or other bone marrow failure diseases who have tiny telomeres or TERT or TERC mutations. Folks with a lung disease (Idiopathic pulmonary fibrosis) are also included in the trial, because TERT mutations are also implicated in that condition, as well as in liver disease.
Danazol was evidently used decades ago to treat folks with Severe Aplastic Anemia with some success. The folks at NIH think that may have been because of this effect on telomeres.
They've invited me to come up to NIH for further screening for the Danazol trial,
which is described here. Several folks on marrowforums are already enrolled in the trial;
they've started talking about their experiences here. So far, they all seem to be aplastic anemia folks with a TERC mutation, instead of MDSers with a TERT mutation. Either way, it will be good to have company if I wind up doing the trial.
Reading about telomeres, it seems that there may be at least two ways that they can mess up bone marrow, though this may be more conjecture than established fact, at this point.
When a stem cell with a short telomere divides incorrectly, that can trigger the internal functions that cause programmed cell death. Producing lots of defective stem cells and other progenitor cells that die young, after a while, can start to create a shortage of stem cells and cut seriously into the production of good, usable blood cells. This seems to be the problem for folks who have telomere-related AA.
The other problem occurs when a short telomere produces a faulty chromosome division that results in a defective stem cell -- and that stem cell doesn't die, but starts reproducing defective copies of itself. Now we have a clonal disorder, like MDS.
The next step is to head up to Bethesda for screening -- something that is likely to happen sometime in November.