
| Home Forums |
|
|||||||
| Drugs and Drug Treatments ATG, Cyclosporine, Revlimid, Vidaza, Dacogen, ... |
 |
|
|
Thread Tools | Search this Thread |
|
#201
|
|||
|
|||
|
Hey Greg
Very very interesting news about the ferritin levels. Bruce is taking wheatgrass tabs too, and his ferritin came down last time, hmmm.
You poor guy, that BMB story is awful. Bruce has had similar awful, and painful experiences with the local hematologist. The last time local doc did it, his specimen wasn't good enough for the second opinion doctors. Bruce had a nurse practioner in the hospital in Portland do another one a few weeks after the local doc's -- an entirely different experience. You are truly brave to have endured what you did. Good news here. Yesterday, on the way back home from our vacation, Bruce had a CBC done, and he is holding his own. Hgb 9.0, it was 9.1 three weeks ago. He's still feeling well, and has even managed to avoid catching this cold that I've had for 2 weeks. You put it very well, the living with uncertainty and waiting for results of blood tests. We tried while on vacation to let that go. We weren't totally successful, but came back recharged. We realized while we were gone how much energy and time we have put into worrying and wondering and doctoring -- and how valuable some time away was. Hugs, Catherine
__________________
Catherine, wife of Bruce age 75; diagnosed 6/10/11 with macrocytic anemia, neutropenia and mild thrombocytopenia; BMB suggesting emerging MDS. Copper deficient. Currently receiving procrit and neuopogen injections weekly, B12 dermal cream and injections, Transfusions ~ 5 weeks. |
|
#202
|
|||
|
|||
|
Going OFF VALTREX
My local dr. and I decided I would go off Valtrex today. I have been over the 200 mark for my CD4 counts for a while now. When I was at the NIH March 1, I was over 200 and they told me to stop Pentamidine and Valtrex. I stopped the Pentamidine, but wasn't comfortable stopping the Valtrex. Now, however,my cD4 count is about 380, so my local dr. and I decided to stop the Valtrex now. I think the Valtrex was causing my LD count to be high and I really don't want that high. My local dr. also feels that being off the Valtrex, might help my CD4 count go even higher, more quickly. also, in response to another question about my immune system, I was told "I have nearly completely recovered your immunity. Just a few lymphocyte populations are low, but none are critically lowquickly."
Did anyone experience any viral problems after going off of Valtrex? I'm nervous, but giving it a try. 
__________________
Dx. 6/08 with AA, then changed shortly thereafter to MDS. Campath trial at NIH March '09 and have been transfussion independent since June '09 |
|
#203
|
|||
|
|||
|
Going OFF VALTREX
My local dr. and I decided I would go off Valtrex today. I have been over the 200 mark for my CD4 counts for a while now. When I was at the NIH March 1, I was over 200 and they told me to stop Pentamidine and Valtrex. I stopped the Pentamidine, but wasn't comfortable stopping the Valtrex. Now, however,my cD4 count is about 380, so my local dr. and I decided to stop the Valtrex now. I think the Valtrex was causing my LD count to be high and I really don't want that high. My local dr. also feels that being off the Valtrex, might help my CD4 count go even higher, more quickly. also, in response to another question about my immune system, I was told "You have nearly completely recovered your immunity. Just a few lymphocyte populations are low, but none are critically low."
Did anyone experience any viral problems after going off of Valtrex? I'm nervous, but giving it a try. 
__________________
Dx. 6/08 with AA, then changed shortly thereafter to MDS. Campath trial at NIH March '09 and have been transfussion independent since June '09 |
|
#204
|
|||
|
|||
|
Quote:
Glad to hear that you guys had a restful vacation. We were scheduled for our annual Spring camping trip to the beach the week I got pneumonia, so that blew up the trip. Not only is that bad because we probably won't be able to go until Fall, it's especially bad because I count on standing for hours on the beach with a fishing rod every spring to cure pasty white leg syndrome at the beginning of shorts season. Your comment about bravery in the face of a nasty BMB reminded me that, when the Sr. doc came in and poked a third hole in me, the nurse helpfully asked "does that hurt? Are you okay?" "I'm fine," said I. "He's stoic," said the Sr. Doc. I thought that pretty funny at the time; it's not a word you hear every day. I've decided that the individual reaction to a BMB is like the individual reaction to a trip to the dentist. Both experiences can be good or bad, of course, but some folks are terrified of them, regardless of actual punishment endured. It's just another little peculiarity that makes us all different. I'm trying some wheatgrass powder now, having gone through my first bottle of tablets. I've been playing around with whizzing it up in a smoothie for mid-morning snack. Take care! Greg
__________________
Greg, 59, dx MDS RCMD Int-1 03/10, 8+ & Dup1(q21q31). NIH Campath 11/2010. Non-responder. Tiny telomeres. TERT mutation. Danazol at NIH 12/11. TX independent 7/12. Pancreatitis 4/15. 15% blasts 4/16. DX RAEB-2. Beginning Vidaza to prep for MUD STC. Check out my blog at www.greghankins.com |
|
#205
|
|||
|
|||
|
Hey Lisa!
Congrats on the big lymphocyte count and for kicking the Valtrex. I hope it goes off without a hitch. Take care, Greg
__________________
Greg, 59, dx MDS RCMD Int-1 03/10, 8+ & Dup1(q21q31). NIH Campath 11/2010. Non-responder. Tiny telomeres. TERT mutation. Danazol at NIH 12/11. TX independent 7/12. Pancreatitis 4/15. 15% blasts 4/16. DX RAEB-2. Beginning Vidaza to prep for MUD STC. Check out my blog at www.greghankins.com |
|
#206
|
|||
|
|||
|
Hi Greg,
You really are a hero. I wouldn't have said I was fine in that situation. And you've definitely passed the good attitude test. If you get a trainee next time, I hope they give you something to knock you out!! Fishing at the beach is heaven, isn't it? I'm sorry you missed your trip this spring. Speaking of the pneumonia, are you completely through with that? Cheers, Catherine
__________________
Catherine, wife of Bruce age 75; diagnosed 6/10/11 with macrocytic anemia, neutropenia and mild thrombocytopenia; BMB suggesting emerging MDS. Copper deficient. Currently receiving procrit and neuopogen injections weekly, B12 dermal cream and injections, Transfusions ~ 5 weeks. |
|
#207
|
|||
|
|||
|
Hey Catherine!
Yep, the Pneumonia never really amounted to anything. I never even had a cough. I guess the pleurisy that one night was a good alarm that got me the antibiotics quickly, and that wiped out the pneumonia lickety-split. The emergency room visit, complete with CT Scan, also wiped out my health insurance deductible lickety-split. I think the doc was being extra careful because I showed him my offiicial-looking NIH letter about not having a great immune system and being susceptible to PCP pneumonia. Had it not been for that, he'd have probably just prescribed the antibiotics and sent me home without the scan. But those CT Scans are not cheap! Take care! Greg
__________________
Greg, 59, dx MDS RCMD Int-1 03/10, 8+ & Dup1(q21q31). NIH Campath 11/2010. Non-responder. Tiny telomeres. TERT mutation. Danazol at NIH 12/11. TX independent 7/12. Pancreatitis 4/15. 15% blasts 4/16. DX RAEB-2. Beginning Vidaza to prep for MUD STC. Check out my blog at www.greghankins.com |
|
#208
|
|||
|
|||
|
NIH Campath Trial -- Six Month BMB
They say that no news is good news, though that's not necessarily a comforting thought for those of us in the news business.
It may well be the truth when it comes to the results of my recent bone marrow biopsy at NIH. The procedure was part of the six-month follow-up and is the first biopsy I've had since October, during my screening appointment for the Campath trial. I don't have the actual lab reports in hand, just a brief email from Dr. Matt Olnes, but the news is both boring and encouraging: no change. My marrow is normo-cellular, with trilineage dysplasia, less than five percent blasts, and the same abnormalities as seven months ago: trisomy 8 and a duplication in the long arm of chromosome 1 in a percentage of the cells analyzed. Why is no change good news? In the theory behind the Campath trial, we aren't trying to fix or kill the abnormal stem cells. We were trying to stop the autoimmune war in my bone marrow that had my T-cells attacking my stem cells -- a war that may have caused the abnormalities in the first place. The risk -- and what I feared this biopsy might reveal -- is that the aberrant stems cells, the "clone," would continue to evolve, taking on additional mutations, like monosomy 7 or other higher-risk abnormalities that might signal the disease is progressing. Or the biopsy might have shown a growing percentage of blasts, another scary development. But the biopsy showed none of this. That suggests there is currently a cease-fire underway in my marrow, and my blood-producing factory is having a chance to rebuild. And, in fact, all my counts are up compared to their level when I entered the trial, with the exception of hemoglobin, which is why I still need red cell transfusions every four weeks. And the solution to that problem, we hope, is a matter of time. These results cement my resolve to remain in the trial, and wait for improvement. The one question that Dr. Olnes' email did not reveal -- but that I hope to have the answer to next week -- is whether the percentage of abnormal stem cells has increased significantly. Past biopsies have pegged the percentage at roughly fifty percent. The lab folks only look at twenty cells to do this analysis, so the percentages have to be taken with a grain of salt. But finding that all of my cells now have the abnormalities would be a cause for concern. On the other hand, even that would not change my decision about waiting giving my marrow longer to heal.
__________________
Greg, 59, dx MDS RCMD Int-1 03/10, 8+ & Dup1(q21q31). NIH Campath 11/2010. Non-responder. Tiny telomeres. TERT mutation. Danazol at NIH 12/11. TX independent 7/12. Pancreatitis 4/15. 15% blasts 4/16. DX RAEB-2. Beginning Vidaza to prep for MUD STC. Check out my blog at www.greghankins.com |
|
#209
|
|||
|
|||
|
Hi Greg, I hope you continue to improve your counts, and wow you lost 30-40 pounds, congratulations! I had a similar experience with my diet changes which are based on a few of the books you suggested. I wound up following the Dean Ornish spectrum book which made the most sense to me. I stick to his most healthy choices which eliminates sugar, meat, processed foods etc.. I have had allergies my whole life been tested and did allergy shots which reduced but never eliminated them but for some reason they are now gone. I just had a cbc done the other day and my numbers were stable which is what I was hoping for. I have to ask what did you decide to do diet wise? I sure you have some great insights based on your research.
__________________
Tom- 62 yrs old, dx-eosinophilic fasciitis 2004, 1 yr prednisone resolves EF- now low counts, HGB has been ok... EF has been associated with MDS along with AA. |
|
#210
|
|||
|
|||
|
Hi Greg,
It's great that everything is going according to plan (except for your hgb not coming up as fast as hoped). I know there have been a lot of ups and downs the past 6 months for you -- boring can be very good.  Also good to be able to make a decision about continuing on the trial. Also good to be able to make a decision about continuing on the trial.Hugs, Catherine
__________________
Catherine, wife of Bruce age 75; diagnosed 6/10/11 with macrocytic anemia, neutropenia and mild thrombocytopenia; BMB suggesting emerging MDS. Copper deficient. Currently receiving procrit and neuopogen injections weekly, B12 dermal cream and injections, Transfusions ~ 5 weeks. |
|
#211
|
|||
|
|||
|
Hey Tom!
Hey Tom!
Sorry for the slow response. Things got nuts around here and I missed your post. I'm not sure I'm a good one for recommending diets: I tend to incorporate a lots of ideas I pick up here and there, though only if they strike me as common-sensical. What strikes me as common-sensical is usually stuff that makes sense if you think about what the diet of humans might have looked like as hunter-gatherers and early agriculturalists, when our food was shaping us as a species more than we were shaping our food. (I think I picked up this idea from Bill Phillips' Body for Life, among other places.) I'm skeptical of diets that seem like they are the product of too much theorizing. So, what I've done since being diagnosed is a real hodge-podge. I gave up alcohol, because my transplant doc told me to. That probably accounts for more of the weight loss (which has been 30 lbs.; I'm aiming for 15 more). I eat less than I used to -- but more frequently. Bigger breakfast and supper; two small meals in the middle of the day. I eat less meat and more vegetables. And I eat much, much more fruit. Servan-Schreiber in his book Anti-Cancer talks about a French study that found significant reduction in breast cancer among women who ate a wide variety of fruit. I figure having lots of different anti-oxidants running around inside me is a good thing. Which fruits tends to vary by season, though I use frozen berries in my smoothies. I plan to freeze my own blueberries in the next few weeks, as well as the wild blackberries I gather in the neighborhood. We have a garden, so, particularly in the summer, we have lots of fresh, organic vegetables. We have chickens, so I eat a lot of eggs. I also have chicken in the freezer that I raised myself. I plan to start getting my beef and pork from the growing number of local folks who are raising these in the older grassfed and pastured tradition; I'm working on a source (and on making room in the freezer!) I don't eat a ton of grains, but go for whole grains when I do (except for jasmine rice, for which I have a weakness). Despite not making meat the centerpiece of everything, I still make it a point to get plenty of protein. I drink lots of green tea, lots of water, two cups of coffee every morning, and no soda at all. I have 2.5 oz of 85% dark chocolate most every evening. I exercise an hour every morning -- a combination of stationary bike and strength training (weight bench and dumbbells). I've just started tracking my food and fitness using MyPlate at livestrong.com, because I've decided to get down to 165 and lose the remnants of my paunch. That's all highly disorganized, I know. But it's where I am at the moment. I have a high tolerance for other folks' choices on all this. One of my daughters is a vegan; the other is a dedicated carnivore with a taste for good wine and cheap beer. As Michael Pollan says, human beings are capable of existing pretty darned well on a wide range of diets -- including mostly walrus blubber. The only diet known to be truly toxic to humans is the standard modern Western diet. On the other hand, those of us with weird bone marrow probably need to be a little more attentive than the average Joe. Hope all is going well for you -- it sounds like you are doing fantastic. Take care! Greg
__________________
Greg, 59, dx MDS RCMD Int-1 03/10, 8+ & Dup1(q21q31). NIH Campath 11/2010. Non-responder. Tiny telomeres. TERT mutation. Danazol at NIH 12/11. TX independent 7/12. Pancreatitis 4/15. 15% blasts 4/16. DX RAEB-2. Beginning Vidaza to prep for MUD STC. Check out my blog at www.greghankins.com |
|
#212
|
|||
|
|||
|
NIH Campath Trial -- Six Month BMB (Cytogenetics)
I've been negligent about reporting on the more detailed results of my six-month bone marrow biopsy. Fortunately, that negligence is more about being busy than avoiding the results, which were, frankly, pretty boring.
You might remember that the biopsy itself was pretty exciting, involving two docs, three holes in my backside, and difficulty extracting the actual marrow sample. After all of that drama, the pathologist's report drily remarked that the marrow sample was small, crushed, and inadequate for analysis. So, we have no new info on that front. The liquid portion of the sample was adequate for analysis, but produced results not much more interesting: no change. Now, some folks might be disappointed with "no change" six months along in a course of treatment. But I was actually pretty pleased. The greatest worry I had going into this six month checkup was that the BMB would find something nasty -- like an increased blast count or a Monosomy 7 abnormality -- that would suggest disease progression and force me to consider more aggressive therapy. Fortunately, that didn't happen. The principal investigator's conclusion? "Overall it looks the same as prior to treatment." There was, however, a change in my cytogenetics that taught me something new about that particular analysis. The overall percentage of abnormal cells revealed in the analysis increased, but neither the pathologist nor Dr. Matt Olnes, the principle investigator on the trial, found that worrisome -- or even significant. It turns out that "Metaphase karyotyping isn't a strictly quantitative test because of the few numbers of cells analyzed," according to Dr. Olnes. This makes sense to me, as someone with a just enough understanding of statistics to be dangerous. After all, you can't stop 20 people on the street, ask them who's going to win the next election, and figure you have the answer nailed down. You have to have a much larger sample to produce statistically significant results. Back in September 2010, the results of my last biopsy at Wake Forest University showed 55 percent abnormal cells and 45 percent normal. All of the abnormal cells showed both a duplication in the long arm of chromosome 1 and three copies of chromosome 8 (Trisomy 8). Roughly a month later, my screening BMB at NIH showed 55 percent of my cells with the dup1q abnormality, but only 30 percent of those cells with Trisomy 8. My latest BMB showed 83 percent abnormal cells: all of those had the dup1q, but only 13 percent also had Trisomy 8. When I brought this to Dr. Olnes attention, he replied, "We do see patients who show fluctuation in their clone sizes by cytogenetics who are otherwise stable." So, absent some change in my actual symptoms, he didn't really see the change in percentage as significant. That judgement would be different if some new abnormality had cropped up, of course. But, for now, things are essentially unchanged. And "unchanged" is, in my mind, something of a relief.
__________________
Greg, 59, dx MDS RCMD Int-1 03/10, 8+ & Dup1(q21q31). NIH Campath 11/2010. Non-responder. Tiny telomeres. TERT mutation. Danazol at NIH 12/11. TX independent 7/12. Pancreatitis 4/15. 15% blasts 4/16. DX RAEB-2. Beginning Vidaza to prep for MUD STC. Check out my blog at www.greghankins.com |
|
#213
|
|||
|
|||
|
Hey Greg,
That is a bummer that after that painful experience you went through training a doctor in how to do a BMB, it isn't usable. But also very interesting how Dr. Olnes analyzed the information he got. We tend to get so focused on every little variation in the labs -- this was a good reminder than statistical variations must also be considered. On another subject, have you had a urinary copper excretion test? Regards, Catherine
__________________
Catherine, wife of Bruce age 75; diagnosed 6/10/11 with macrocytic anemia, neutropenia and mild thrombocytopenia; BMB suggesting emerging MDS. Copper deficient. Currently receiving procrit and neuopogen injections weekly, B12 dermal cream and injections, Transfusions ~ 5 weeks. |
|
#214
|
|||
|
|||
|
Quote:
I have not had this, though I have read a bit of the exchange between you and Chirley about it. Is the point to see whether I'm just dumping all the extra copper I'm taking? Fill me in on why I should have this. Also, I know that you have done much more copper research than I have since I got sidetracked into immunosuppression land. But, as I say in a post I haven't quite finished yet, I'd like to get my RBC factory tuned up a bit. And I gather from your posts that Bruce sees a difference in transfusion requirements when his copper is in the 60s vs the 80s. All the stuff I've read deals with extremely low copper mimicking MDS, as opposed to marginally low copper impacting transfusion requirements. Have you run across studies that look at the latter? I have a feeling that, if I'm going to work on copper, it's going to have to be with my family doc. Take care! Greg
__________________
Greg, 59, dx MDS RCMD Int-1 03/10, 8+ & Dup1(q21q31). NIH Campath 11/2010. Non-responder. Tiny telomeres. TERT mutation. Danazol at NIH 12/11. TX independent 7/12. Pancreatitis 4/15. 15% blasts 4/16. DX RAEB-2. Beginning Vidaza to prep for MUD STC. Check out my blog at www.greghankins.com Last edited by Greg H : Sun Jul 3, 2011 at 10:51 PM. Reason: typo |
|
#215
|
|||
|
|||
|
BMB - Greg
Greg - you likely had the same fellow do your BMB as I had. At least in my last one, he got enough, even though it was a very small sample. That was after a very long BMB, probably 45 min- 60 minutes (some of which was quite painful) I hope next year is better!!!
__________________
Dx. 6/08 with AA, then changed shortly thereafter to MDS. Campath trial at NIH March '09 and have been transfussion independent since June '09 |
|
#216
|
|||
|
|||
|
NIH Campath Trial -- Six Month Conclusions
So, where do we go from here?
I was already inclined, based on my conversation with Dr. Matt Olnes and the other folks at NIH during my six-month follow-up, to continue waiting for my marrow to recover, post-Campath, rather than moving to some other therapy. After getting my detailed bone marrow results, my inclination hasn't changed. There's no dramatic change, so I see no reason to jump ship now. Everything I've read on marrowforums from folks with MDS or AA who've had immunosuppression says it takes a while for the marrow to heal; I'm going to give mine some time to heal. Besides, there are some positive signs. Between diagnosis, in March 2010, and beginning the Campath trial, in November my platelets slid from the high 90s to the high 60s. The trend was pretty persistent, and not in a positive direction. My last two CBCs have pegged my platelets over 100. My white blood cell and neutrophils counts had undergone a similar slide. The Campath kicked a hole in my WBC and neutrophil counts, of course, but they continue to improve, and the neutrophils have nearly reached pre-Campath levels. So, it's not like, from my perspective, there's been no improvement here. Things were headed in the wrong direction; now some things seem headed in the right direction. The exception, of course, is my need for red blood cell transfusions. I was being transfused every six weeks before Campath; I'm still getting RBCs every four weeks now. So, while I'm waiting around for things to improve, I'm going to start working a little harder on finding out what I can do to help out the RBC factory in my marrow. Here are some thoughts: IRON - doesn't seem to be a problem. If anything, I've got too much of that, based on my monthly transfusions, and the BMB showed "increased" iron stores in my marrow. I'm continuing the wheatgrass to try to chelate some iron without resorting to the expensive pharmaceutical alternative Exjade. Neither Principal Investigator Matt Olnes nor my local hematologist have recommended chelation at this point, based on the available research on its value for MDS patients. I know a lot of folks on marrowforums are on Exjade or other chelators; I'd be interested in understanding why. COPPER - My copper was marginally normal (71) when I was diagnosed. I've been taking 6mg of chelated copper every day for 15 months, and my copper has been as low as 46 and as high as 70. It was 66 at last check. Clearly, I'm not making progress. The nutritionist at Wake Forest provided information that suggested oral copper should be taken with zinc to aid absorption. But, back in November, the docs at NIH had me continue the copper while dropping the zinc, probably relying on research that shows too much zinc can result in a copper deficiency. Dr. Olnes reiterated that advice the other day, concerned that too much zinc could hurt copper absorption and doubtful that a smaller dose would help it. Both he and my local hematologist suggested upping my oral dose to 9 mg per day. I think I am going to find a good no-iron multivitamin that has an mg or two of copper and maybe 15 mg of zinc and take that to increase both copper and zinc. I'm not currently taken a multivitamin (never have). EPO - I had my EPO levels checked early on, and it was way over the level that makes an ESA a reasonable option. I'm not sure if EPO levels change over time, but it seems like a reasonable question to ask my local hematologist, to see if a retest is reasonable. ESAs are not part of the Campath protocol, so, even if my EPO made an ESA an option, I wouldn't make a move in that direction until November. But, still, I'd like to know. SUGGESTIONS? - I'm interested in figuring out whatever else I can do to help out my red blood cell factory. B12 was 466 a year ago; 1016 in October. Folate is way above the low end of normal. I'm taking both. I'd be interested in any thoughts you all have. Take care! Greg
__________________
Greg, 59, dx MDS RCMD Int-1 03/10, 8+ & Dup1(q21q31). NIH Campath 11/2010. Non-responder. Tiny telomeres. TERT mutation. Danazol at NIH 12/11. TX independent 7/12. Pancreatitis 4/15. 15% blasts 4/16. DX RAEB-2. Beginning Vidaza to prep for MUD STC. Check out my blog at www.greghankins.com |
|
#217
|
|||
|
|||
|
Hi Greg
Good questions and ruminations, as usual.
I think Marlene would be a good one to weigh in on your post. Neither we nor the doctor have been able to find much research about slightly to moderately low level copper and the effect on red blood cell production. We have noticed that when Bruce's copper level has gotten into the normal range, stabilization of his red blood counts occurs a few weeks later. Also, when his copper level drops, there is a delayed reaction to the drop in rbc, also about 2-3 weeks. This is not a research finding, of course. He was supplementing 10 mg day of chelated copper for 2 months, without his serum copper level or ceruloplasmin increasing significantly. After the IV injections of copper sulfate began, his copper level rose quickly to the mid 80's. Bruce also began herbal chelation to address his high ferritin levels, as well as wheatgrass supplementation. Bruce also continued to take 10 mg/day of oral copper. After the initial spike into normalcy, the last 2 copper tests have been below normal, despite increasing the frequency of the IV injections to 2x/week. We have not discussed the urine excretion findings with the doctor yet -- have an appt with him next week. After the nurse told Bruce about the high excretion rate of copper in Bruce's urine, we wondered whether there might be a connection between the high excretion rate, and the chelation and wheatgrass supplementation. So until he talks to the doc, Bruce has discontinued herbal chelators and wheatgrass. As an aside, we also don't know about the potency or efficacy of the oral copper supplements Bruce was taking. After reading Chirley's posts, I tried to find a source here for tincture of copper sulfate. Our compounding pharmacies say they cannot create it. I found a supplier for a liquid copper sulfate tincture online. Ordered some and it arrived the temperature of a hot bath, along with a warning to keep it cool and dry.  Bottom line -- we don't know yet how much a role the copper level plays in Bruce's anemia. But he would like to get it into normal range long enough to rule it in or out as a factor. So, the journey continues. Cheers, Catherine
__________________
Catherine, wife of Bruce age 75; diagnosed 6/10/11 with macrocytic anemia, neutropenia and mild thrombocytopenia; BMB suggesting emerging MDS. Copper deficient. Currently receiving procrit and neuopogen injections weekly, B12 dermal cream and injections, Transfusions ~ 5 weeks. Last edited by cathybee1 : Thu Jul 7, 2011 at 05:47 PM. |
|
#218
|
|||
|
|||
|
Hi Greg, for what it is worth... I'm in watch and wait so I want to do something to try to get my numbers closer to normal range. I read a number of books, some that you suggested and did some basic a scoring on what diet might stack the deck in my favor. I settled on the Dean Ornish program and have been making changes to get on his full reversal diet by the end of the summer. His program has success in heart disease, prostate cancer and gene expression. I gave up meat, sugar, processed foods and I'm working on reducing the amount of fruit in my diet ( I also gave up milk products while ornish doesn't have an issue with no fat milk, the china study was bugging me so that was throw out also). I'm not on his full reversal diet yet as I have salmon 3 times a weeks and I still have some almonds,walnuts and avocado as well as more that 5 servings of fruit. I would say I'm about 90% on the reversal program. My last blood work was stable which I was glad I didn't kick a hornets nest by making a big diet change. I'm not concerned with my b12 right now as I'm getting that checked often and it been on the high side.
I do not have a success story on this yet other than my life long allergies going away and dropping 30lbs (I dropped the 30lbs and have stayed at that weight). I wanted to try something that Bruce and Marla over at aplastic central have discussed but settled on this. I'm pretty sure my issue is related to my past autoimmune history. I took out the books but most of the reversal diet and information on his trials are on his web site.
__________________
Tom- 62 yrs old, dx-eosinophilic fasciitis 2004, 1 yr prednisone resolves EF- now low counts, HGB has been ok... EF has been associated with MDS along with AA. |
|
#219
|
|||
|
|||
|
Quote:
Thanks for that great update. "not a sexy area for research" seems to be a problem where MDS is concerned. Dr. Olnes said we really need a good prospective study of iron chelation in MDS, and then opined that no one is likely to do one. I'm awaiting a copper level from Tuesday's blood draw; should have it sometime next week. I was worried about going up to 9mg of oral copper, but, if Bruce is doing 10mg, maybe I shouldn't worry I do have the same questions about chelation that you have: If the wheatgrass is chelating iron, is it chelating copper as well? And I haven't found anything that resembles an answer. What was the herbal chelator Bruce's doc had him taking? I may want to give it a shot. I'll be interested to learn what Bruce's doc has to say about the high levels of excreted copper. Thanks much! Greg
__________________
Greg, 59, dx MDS RCMD Int-1 03/10, 8+ & Dup1(q21q31). NIH Campath 11/2010. Non-responder. Tiny telomeres. TERT mutation. Danazol at NIH 12/11. TX independent 7/12. Pancreatitis 4/15. 15% blasts 4/16. DX RAEB-2. Beginning Vidaza to prep for MUD STC. Check out my blog at www.greghankins.com |
|
#220
|
|||
|
|||
|
Hey Tom!
Thanks for the recommendation. I'll check out his website. Giving up fruit gives me pause, because of the antioxidants (and that French study that showed consumption of lots of different kind of fruits inversely correlated with breast cancer), but I imagine he's trying to get rid of sugar and gets the antioxidants in some other way. I'm pretty much out of processed foods, aside from shredded wheat occasionally in the morning, but I definitely eat some meat, lots of eggs, and reasonable amounts of cheese and butter. My wife doesn't do fish, so I don't either, even though I'm a fan. Fortunately, despite a family history of heart disease and diabetes, I don't seem to have acquired those tendencies. It's just the MDS with me. I appreciate the thoughts! Greg
__________________
Greg, 59, dx MDS RCMD Int-1 03/10, 8+ & Dup1(q21q31). NIH Campath 11/2010. Non-responder. Tiny telomeres. TERT mutation. Danazol at NIH 12/11. TX independent 7/12. Pancreatitis 4/15. 15% blasts 4/16. DX RAEB-2. Beginning Vidaza to prep for MUD STC. Check out my blog at www.greghankins.com |
|
#221
|
|||
|
|||
|
Hi Greg, I'm still fine tuning my diet but based on what I understand now I eat too many servings of fruit a day. It's the sugar that is the issue, I just asked a question on that site that gives some further information. I was making a veggie smoothie that I call the 'exorcist' I'm pretty sure it might be what they used in the movie. Anyway it had at least 16 oz of OJ in it and I was drinking 2 a day sometimes. Spinach carrots broccoli and OJ in the smoothie along with lots of other fruit during a day so I'm going to cut that back to a more normal amount.
Here is the dialog on the Ornish site... Default fruit juice Hi, what group do different quantities of fruit juice (organic OJ specifically) fall into if it's over 8 oz as specified in the group 1? for example if I drink 16oz is that considered group 2? if I drink more does at what point does it go into group 5? Thanks __________________ Tom Edit/Delete Message Reply With Quote Multi-Quote This Message Quick reply to this message #2 Report Post Old 07-02-2011, 02:01 PM PMRI Moderator PMRI Moderator is offline Administrator Join Date: Dec 2008 Posts: 216 Default Hi, Tom! You ask an excellent question! In the Dr. Dean Ornish Program for Reversing Heart disease, fruit and fruit juices are limited to 2-4 servings per day (approx 26gms carbohydrate/cup). For example, one serving of a fruit juice is considered ½ cup. So if you are drinking 16 oz of OJ per day, you are essentially drinking your allotted daily fruit servings. [Serving size is an excellent way to look at food portions differently and an important concept to learn if one wishes to lose weight.] At what point OJ becomes a Group 5 food? Is it when you consume more than the recommended servings of fruit per day, or in your case 16 oz.? I think it depends on who you are, how you eat, whether you consume this amount of OJ every day versus once a week, any medical conditions, and your risk profile such as being overweight, etc. In The Spectrum, Dr. Ornish states that any healthy food can become less healthy if consumed in high quantities. The caveat about consuming fruit juices (and perhaps what you may be referring to), in lieu of the natural fruit, is that fruit juices contain high amounts of fructose, even when there is ‘no sugar added,’ and are low in fiber. Therefore, drinking fruit juice causes a rapid rise in blood sugar, which causes a surge in insulin secretion. Over time, these surges can predispose one to insulin resistance, impaired glucose intolerance and even impaired lipid metabolism (high triglycerides, lower LDL particle size), all of which are precursors to type 2 diabetes and metabolic syndrome. There is a slower rise in blood sugar when eating the actual fruit due to its fiber content (slows absorption in the gut and also feels more 'filling'). Also, fruit juice is more concentrated that the actual fruit, and therefore, higher in calories – an issue if you are trying to lose weight.
__________________
Tom- 62 yrs old, dx-eosinophilic fasciitis 2004, 1 yr prednisone resolves EF- now low counts, HGB has been ok... EF has been associated with MDS along with AA. |
|
#222
|
|||
|
|||
|
MyeloMud
Hey Tom!
This makes sense about the OJ. I've read elsewhere on this glucose intolerance stuff. I've been doing a smoothie in order to take my wheatgrass everyday. I started out with a 50/50 combo of 1/2 cup pomegranate and 1/2 cup apple juice, but that was too sweet and pretty high in calories. I picked up some Bolthouse carrot juice at the grocery and substituted it for the apple juice. I'm not sure I'd want to drink it straight, but it was just the trick for the smoothie. It cuts down on the sweet, sugar, and calories. My "MyeloMud" recipe goes like this: 1/2 cup carrot juice 1/2 cup pomegranate juice 1/4 cup frozen berries (I use blackberries or black raspberries I picked, local blue berries I froze, or the frozen store-bought equivalents). 1 scoop wheatgrass powder 2 scoops vanilla NatureAde whey protein powder 6 ice cubes I whiz all that up in a blender. The whey protein powder creates a much nicer whipped consistency than the soy protein powders I've tried. It winds up looking like this. [IMG]  IMG_1115 by hankins.greg, on Flickr[/IMG] I don't actually measure the Pom and Carrot every time. I more just eyeball it. If you get a little too much carrot, it tends to look brown instead of purple. And this batch was with blackberries, which make it more purple than do the blueberries. I entered the recipe into Livestrong and here's the nutritional chart I got back: [IMG] 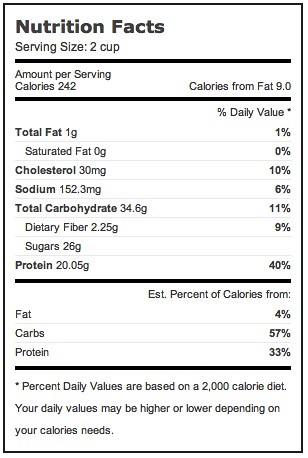 Nutrition by hankins.greg, on Flickr[/IMG] I noticed when I entered the recipe that the carrot juice has less than half the calories of the pomegranate juice. This smoothie is definitely more tart than sweet. You might want to try the carrot juice to sub in for some of your OJ. The Bolthouse brand is $4.98 a quart at my grocery, but you can get two quarts for $5.98 at Sam's Club. And I only use 1/2 cup a day. The Pom is even more expensive, but, again, a quart lasts me a while. Take care! Greg
__________________
Greg, 59, dx MDS RCMD Int-1 03/10, 8+ & Dup1(q21q31). NIH Campath 11/2010. Non-responder. Tiny telomeres. TERT mutation. Danazol at NIH 12/11. TX independent 7/12. Pancreatitis 4/15. 15% blasts 4/16. DX RAEB-2. Beginning Vidaza to prep for MUD STC. Check out my blog at www.greghankins.com |
|
#223
|
|||
|
|||
|
Quote:
I always wondered if sleeping in a high-altitude chamber could help with increasing RBCs in bone marrow failure patients. I think it works by stimulating your EPO though. Maybe there are other blood doping techniques used by athletes that could be effective for increasing RBC production in MDS patients.
__________________
55 yo female, dx 9/08, AA/hypo-MDS, subclinical PNH, ATG/CsA 12/08, partial response. small trisomy 6 clone, low-dose cyclosporine dependent |
|
#224
|
|||
|
|||
|
Doping
Hey Hopeful!
Very interesting -- and highly appropriate to be thinking about athletic doping, since we're in the midst of the Tour de France. I didn't know that the high-altitude thing was a natural way to increase EPO. Mine tested high previously, so it might not help, but I do plan to see about having it tested again. If I'm going for the high-altitude thing, though, I might prefer a nice six-month vacation in Aspen. I'll have to speak with my boss and insurance company to see if I can work that out!  Take care! Greg
__________________
Greg, 59, dx MDS RCMD Int-1 03/10, 8+ & Dup1(q21q31). NIH Campath 11/2010. Non-responder. Tiny telomeres. TERT mutation. Danazol at NIH 12/11. TX independent 7/12. Pancreatitis 4/15. 15% blasts 4/16. DX RAEB-2. Beginning Vidaza to prep for MUD STC. Check out my blog at www.greghankins.com |
|
#225
|
|||
|
|||
|
I like that idea because I remember my retic count went up after fishing at 7500 feet for a weekend. I asked Dr. Maciejewski this question when I saw him in March, and he didn't think it would be helpful. Others may have a different opinion, so it won't hurt to ask.
__________________
Dallas, Texas - Age 81 - Pure Red Cell Aplasia began March 2005 - Tried IVIG - Then cyclosporine and prednisone. Then Danazol, was added. Then only Danazol . HG reached 16.3 March 2015. Taken off all meds. Facebook PRCA group https://www.facebook.com/groups/PureRedCellAplasia/ |
 |
| Thread Tools | Search this Thread |
|
|
 Similar Threads
Similar Threads
|
||||
| Thread | Thread Starter | Forum | Replies | Last Post |
| Pilot study of Alemtuzumab (Campath) at NIH | Barbara2007 | Clinical Trials | 9 | Thu May 5, 2022 12:38 AM |
| New Promacta (Eltrombopag) Clinical Trial at NIH | Sally C | Clinical Trials | 73 | Sun Dec 30, 2018 05:52 AM |
| NIH Trial - Plt Count Level Feedback/Experience | disco3md | AA | 1 | Wed Jun 28, 2017 01:08 PM |
| NIH Trial (Eltrombopag & Cyclosporine) | disco3md | Clinical Trials | 0 | Mon Jun 26, 2017 05:02 PM |
| Subcutaneous Campath Trial | Nadia T | Clinical Trials | 3 | Fri Dec 20, 2013 09:06 PM |