
| Home Forums |
|
|||||||
| Drugs and Drug Treatments ATG, Cyclosporine, Revlimid, Vidaza, Dacogen, ... |
 |
|
|
Thread Tools | Search this Thread |
|
#76
|
|||
|
|||
|
NiH Campath Trial Day 11
Happy Thanksgiving! Day 11 of the NIH Campath trial was almost uneventful, except for the reappearance of a mysterious and ephemeral rash on my behind, and the return visit of daughter Jeni and her true love Billy. There is no evidence that the rash and visit are related, I hasten to add.
Back on Day 8, on the way to my first pentamidine treatment (which was so uneventful I forgot to write about it; see the update below), I discovered an odd rash on my hips. I went ahead with the pentamidine; but, upon my return to the unit, I showed my nurse the rash, a collection of dime-sized raised areas along the outsides of my behind and along my waistline on my back. She expressed surprise at their appearance and went to find the doctor. By the time he arrived, thirty minutes later, they were gone. The next day, no rash. Day 9, I had the rash again, though in a milder outbreak, shortly after showering. I suspected the Dial brand soap provided by the Clinical Center and asked my daughter to pick up some Irish Spring (my usual brand) on her way in to visit. This morning I used the Irish Spring and had a worse outbreak -- more widespread up my back, and itchier. The same nurse was on duty. She took one look and ran for the doctor, who arrived with the attending doc and whole team of fellows. Having lost the coin toss and wound up with Thanksgiving duty, thereby missing the Macy's Thanksgiving Day Parade, they were all too happy to inspect the rash on my behind as a substitute if not entirely equivalent diversion. After I explained the failure of my soap experiment, the attending, Dr. Tisdale, said, "It's probably something we're giving you [i.e., the Campath or the Valtrex], but it's not bad enough that we're going to stop giving you what we're giving you." I typically have the Valtrex early in the morning, but I can't swear I've always had it before the appearance of the rash. However, that does seem like the most logical explanation. Time, I expect, will tell. My counts continued to be excellent today, with only a 0.3 fall-off in Hgb, to 9.2, while platelets are now up to 58 and neutrophils battled back to 1.62. My neutrophils are currently higher than they were when I walked in the door. Tomorrow brings my last dose of Campath, and a busy day: contributing lots o' blood to the phlebotomists, getting rid of the PICC line, having another ECHOcardiogram, and getting fitted with a 24-hour Holter monitor that I will mail back. And then, I will bid a fond farewell to this place and gird myself for a six-plus hour ride to North Carolina and home.
__________________
Greg, 59, dx MDS RCMD Int-1 03/10, 8+ & Dup1(q21q31). NIH Campath 11/2010. Non-responder. Tiny telomeres. TERT mutation. Danazol at NIH 12/11. TX independent 7/12. Pancreatitis 4/15. 15% blasts 4/16. DX RAEB-2. Beginning Vidaza to prep for MUD STC. Check out my blog at www.greghankins.com |
|
#77
|
|||
|
|||
|
NiH Campath Trial Day 8 - Pentamidine Addendum
My experience with Pentamidine on Day 8 was so unremarkable that I forgot to remark on it.
This is an inhaled drug that I'll be taking monthly for a while to fight off any potential infection by Pneumocystis jirovecii, a particularly nasty fungus that is responsible for a particularly nasty pneumonia called "Pneumocystis." A lot of folks walk around with this bug in their lungs, but their immune system keeps it in check. Folks with damaged CD4 T cells -- e.g., folks with AIDS, folks who have taken Campath -- need extra protection. So, we breathe in Pentamidine once a month. The nurse administering the drug mixes it up and puts it into an inhaler called a "nebulizer," which turns the stuff into a fine mist. The patient breathes that mist in through the mouth, exhaling through nose or mouth. Pentamidine reputedly takes like the inside of a tire, makes some folks nauseous, and makes others spit. For me, it was none of the above. I read my book for 20 minutes while inhaling the stuff and then went on my merry way. I just hope it works!
__________________
Greg, 59, dx MDS RCMD Int-1 03/10, 8+ & Dup1(q21q31). NIH Campath 11/2010. Non-responder. Tiny telomeres. TERT mutation. Danazol at NIH 12/11. TX independent 7/12. Pancreatitis 4/15. 15% blasts 4/16. DX RAEB-2. Beginning Vidaza to prep for MUD STC. Check out my blog at www.greghankins.com |
|
#78
|
|||
|
|||
|
Greg,
My wife had routine pentamidine inhaler treatment too. I remember it being unremarkable and uneventful. I didn't even know that some people found the treatment hard to take. Perhaps if the pulmonary technician had told us "this is gonna taste really really bad" then the power of suggestion might have made us believe it! |
|
#79
|
|||
|
|||
|
lymphocyte question
Hi Greg,
Congratulations on your good response to Campath! I was looking at your graphs on lymphocyte count. Do they refer to absolute lymphocyte count? While getting ATG, my absolute lymphocyte count only went down to 0 on the first day of treatment. It was back at 0.1 on the second day and 0.8 the day after my last day of ATG. Perhaps achieving (and holding) a zero lymphocyte count during treatment differentiates the quick responders from the slow responders (like me)??? I'm wondering if a person's response can be predicted during treatment based on their absolute lymphocyte count. In other words, if the treatment doesn't destroy all of the lymphocytes, is a person more likely to have a slow or partial response? I hope your recovery continues to go well.
__________________
55 yo female, dx 9/08, AA/hypo-MDS, subclinical PNH, ATG/CsA 12/08, partial response. small trisomy 6 clone, low-dose cyclosporine dependent |
|
#80
|
|||
|
|||
|
Hey Hopeful!
Yep, my graphs are absolute lymphocyte counts. Your questions are pretty interesting; I wish I knew the answers. The recent Journal of Clinical Oncology article on the NIH Campath trial includes the following sentence: "Alemtuzumab produces a more profound and persistent lymphopenia compared with ATG, making it attractive in the treatment of autoimmune and inflammatory diseases and lymphoid malignancies and in conditioning regimens for SCT." The lab work that Dr. Elaine Sloand has done related to MDS and immunosuppression evidently suggests that, in at least some patients, the real problem is a subgroup of rogue T-cell lymphocytes attacking certain marrow stem cells. (There's a new article on this in Blood that I haven't gotten to read yet, but will report on as soon as I do.) So kicking the lymphocytes in the head and keeping them down seems to be the key. The fact that the Campath is so good at this is why NIH is doing the trial. And, unlike with ATG, they don't automatically follow up with Cyclosporin. That's only brought in if folks relapse, as a rescue. As you've seen from my graphs, my lymphocytes went down quickly (though not quite to zero on Day 1, and then stayed down. One of the objections to Campath is that it takes a very long time for the lymphocytes to recover, which exposes the patient to the potential for infection from viruses they already have, or new ones they are exposed to. One of the Fellows told me that some folks call Campath "AIDS in a bag," because it leaves your immune system compromised in essentially the same way as an AIDS patient. But, so far, NIH has been good at avoiding new infections amongst folks in the trial. I'm not as smart about ATG as I should be. How many days does the typical ATG treatment last? I do know, looking at the Campath results, that there's a wide variation in time to response. Some folks respond quickly; for others it can take a year. Take care! Greg
__________________
Greg, 59, dx MDS RCMD Int-1 03/10, 8+ & Dup1(q21q31). NIH Campath 11/2010. Non-responder. Tiny telomeres. TERT mutation. Danazol at NIH 12/11. TX independent 7/12. Pancreatitis 4/15. 15% blasts 4/16. DX RAEB-2. Beginning Vidaza to prep for MUD STC. Check out my blog at www.greghankins.com |
|
#81
|
|||
|
|||
|
Quote:
|
|
#82
|
|||
|
|||
|
NIH Campath Trial Day 12
Day 12, the final in-hospital day of the NIH Campath Trial, was very busy, compared to the past few days.
After packing my suitcase in the early morning, I received my last dose of Campath from 10:30 am to 12:30 pm, again without incident, aside from some drowsiness an hour into the process, as likely a side effect of the double-dose of Benadryl as of the Campath. Then it was up to Cardio for a post-trial ECHOcardiogram and down to EKG to be outfitted with a 24-hour Holter monitor to record my heart rhythms on the way home. Back in my room, a nurse outfitted with a fetching pink mask removed all 43 centimeters of PICC Line. I was asked to lie on my back for 30 minutes and then released into the wide world with no dietary restrictions, owing to my mild (not moderate) neutropenia. (However, a nice printout called "Don't Let Your Food Make You Sick" was included in the discharge packet, along with some advice about how to respond to various levels of fever.) Earlier in the day, Dr. Yun stopped by, most excited that my absolute reticulocytes (baby red cells) had jumped from 17 to 54, suggesting that my production of red blood cells could be improving. Dr. Tisdale was optimistic about the same result during rounds, though he cautioned we'd want to see if it it held up in subsequent results. 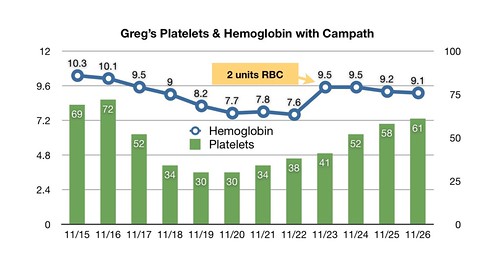 Greg's Hgb & Platelets by hankins.greg, on Flickr Dr. Olnes, the Principal Investigator on the trial, also stopped by for a debriefing. He noted the reticulocyte result and the trend upwards in my platelets. He remarked on the upward trend in my neutrophil count, though he hadn't, at that point, seen that my Day 12 labs showed a steep drop back down to an ANC of 1.32. As I've noted before, neutrophils -- or, at least, my neutrophils -- seem highly variable from day to day. 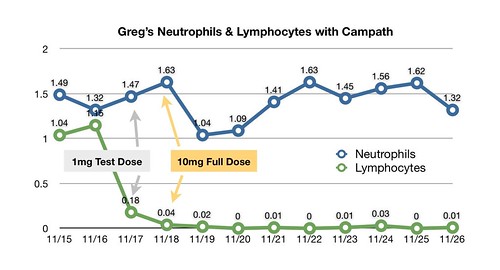 Greg's Neutros and Lymphos by hankins.greg, on Flickr Dr. Olnes also mentioned that Blood had just published a new MDS article by his colleague Dr. Elaine Sloand. It establishes some of the molecular mechanisms underlying the type of MDS that responds to immunosuppressive therapy. It's pretty technical stuff, but I've done my best to summarize the results in a post here. Daughter Jeni and I waited 30 minutes for things to settle down after the removal of my PICC Line; and, after a stop at the pharmacy to pick up a month's supply of Valtrex, we walked past the guards and out the gates of the National Institutes of Health into the next chapter of my life with MDS: waiting for the response. The drive home took longer than I had expected. I'd forgotten that, when pulling an Airstream, 70-miles per hour on the interstate is not a good idea. Given my lack of substantial neutropenia, we even stopped off for dinner at an Olive Garden south of Richmond (It's one of the few national chains at which a vegan can assemble a reasonable meal without feeling out of place. Jeni & Billy are vegans; I'm not definitely not). I'm grateful for all the comments and encouragement I received while in hospital from this wonderful community of teachers, fighters, and survivors. I won't be posting daily results from here on out, since I won't have daily results. (Though I will definitely be following Birgitta's advice to control my temperature morning and evening!) But I do plan to continue to add progress reports to this thread as they become available. I'm scheduled for weekly blood work at my local hematologist's office and a follow-up at NIH in mid-December.
__________________
Greg, 59, dx MDS RCMD Int-1 03/10, 8+ & Dup1(q21q31). NIH Campath 11/2010. Non-responder. Tiny telomeres. TERT mutation. Danazol at NIH 12/11. TX independent 7/12. Pancreatitis 4/15. 15% blasts 4/16. DX RAEB-2. Beginning Vidaza to prep for MUD STC. Check out my blog at www.greghankins.com |
|
#83
|
|||
|
|||
|
It's great to hear everything happened on schedule and your numbers are looking so good. The next part, the waiting, will be much harder, I suspect.
Have a wonderful, delayed Thanksgiving with your family.
__________________
Catherine, wife of Bruce age 75; diagnosed 6/10/11 with macrocytic anemia, neutropenia and mild thrombocytopenia; BMB suggesting emerging MDS. Copper deficient. Currently receiving procrit and neuopogen injections weekly, B12 dermal cream and injections, Transfusions ~ 5 weeks. |
|
#84
|
|||
|
|||
|
Hi Greg
Great that you have completed your trial & stay at the hospital. Wish you all the best in your follow up. Thanks for keeping us posted.
__________________
Lindy 56, low platelets, thrombocytopenia dx 2009, in watch & wait mode. |
|
#85
|
|||
|
|||
|
NIH Campath Trial Week 1 Follow-up
I've been putting off posting the Week 1 follow-up results from my NIH Campath trial both because I've been enjoying a late Thanksgiving and because the Week 1 CBC numbers from my local hematologist's office are pretty much too good to be true.
The schedule for follow-up is two weeks of CBCs and serum chemistries (magnesium, BUN, creatinine, etc.) done locally, plus research tubes overnighted to NIH. Then I'm back to NIH for a day of follow-up, followed by every other week labs locally. Additional one-day trips to NIH are scheduled for three months and six months, when I'll have a bone marrow biopsy. The locally-done CBC from Tuesday found three lymphocytes and 1,200 neutrophils. The latter result is down from the final NIH labs, but I've had problems in the past with the local lab's ANC counts (another reason I was holding this post until I could see the hard-copy report, which I still don't have). Platelets were 68, up from 61 and only one point below where they stood when I started the trial. The too-good to be true part was the hemoglobin and reticulocyte numbers. Hgb stood at 9.5 the day after I had two units of red blood cells at NIH, and had fallen to 9.1 by my last day there. The result from my local clinic was 9.7. On top of that, the reticulocyte count (baby red blood cells) was 157 -- way above normal. If those results are real, then it suggests the red blood cell production factory in my marrow has kicked into gear. But, given the median three months to any response in the trial so far, that's ridiculous. It's a different lab, in a small town, so I'm not getting overly excited at this point. There's a new CBC on Tuesday, and we'll see what that one says before we start jumping up and down. Still, I'm grateful my numbers at least aren't going down. Almost every drug you can take for this crazy disease, including Campath, depresses your counts. So far, I have been very, very lucky on that front, with no platelet transfusions and Hgb that is, at the very least, holding its own. We'll hope for continued good news next week. Interesting side note -- I told the NIH research nurse, Barbara Weinstein, that I was checking my temperature morning and evening. She insisted that I stop -- probably because she thinks it's a bad idea to be obsessing about my disease. "If you feel bad, then check your temperature," she told me. "If you have a fever, go to the emergency room." I didn't mention that spending two weeks in the hospital having your temperature checked four times a day by the nurses is poor training for non-obsession. I figure I'll just be a good patient and follow her advice.
__________________
Greg, 59, dx MDS RCMD Int-1 03/10, 8+ & Dup1(q21q31). NIH Campath 11/2010. Non-responder. Tiny telomeres. TERT mutation. Danazol at NIH 12/11. TX independent 7/12. Pancreatitis 4/15. 15% blasts 4/16. DX RAEB-2. Beginning Vidaza to prep for MUD STC. Check out my blog at www.greghankins.com |
|
#86
|
|||
|
|||
|
Fabulous news, Greg!
__________________
Karen, age 62, dx MDS RAEB-2 1/8/10: pancytopenia WBC 2.7k/Hgb 7.4/Hct 22.1/Plt 19k; complex cytogenetics -3,del(5)(q14q33),-6,+8,+mar,17% blasts. MUD BMT Johns Hopkins 11/30/10. Dx tongue cancer 8/31/12. ok now. blog mausmarrow.com |
|
#87
|
|||
|
|||
|
Greg, that's terrific. Even allowing for differences in lab results, your numbers are still trending the right way.
__________________
Catherine, wife of Bruce age 75; diagnosed 6/10/11 with macrocytic anemia, neutropenia and mild thrombocytopenia; BMB suggesting emerging MDS. Copper deficient. Currently receiving procrit and neuopogen injections weekly, B12 dermal cream and injections, Transfusions ~ 5 weeks. |
|
#88
|
|||
|
|||
|
NIH Campath Trial Week 2 Follow-up
The wise folk on Marrowforums are fond of saying that you best not live by your numbers. This is a good week to take that advice to heart.
After too-good-to-be-true numbers last week, my CBC on Tuesday came up snake eyes, with Hgb down to 8.5 (from 9.7. Yikes!), and platelets down to 53 from 68. My nurse forgot to do the reticulocytes, so I can't report anything on that front. 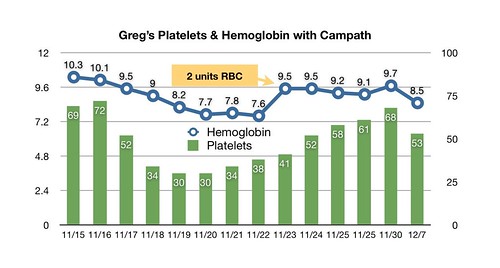 0004ew copy by hankins.greg, on Flickr On the other hand, my immune system continues to be friendly, with absolute neutrophils at 1.16, versus 1.20 last time -- still way above the seriously neutropenic range. And the lab couldn't find any of the lymphocyte stragglers still swimming around in my veins and arteries. I'm back up to NIH on next Tuesday and will be interested to have some numbers from their lab to compare to these from the local lab. I also hope they'll share whatever exotic things they are doing with the tubes of blood I'm sending them weekly -- for example, let me in on what's happening with my cytomegalovirus (CMV) and Epstein-Barr Virus (EBV) counts. On the virus front -- or the potential virus front -- I have had some very strange symptoms this past week. The right side of my chest, along with my shoulder and shoulder blade, have been affected with a burning, prickly pain that comes and goes. It's always there if I touch the affected area but sometimes has a real fit all on its own and becomes irritating enough to make me testy -- even without any touching. I actually noticed this sensation right after I left NIH, but thought it was skin irritation brought on by the EKG tech dry-shaving some hair off my chest when he placed the Holter monitor leads. Then I thought maybe it was some nerve irritation brought on by the bibbed overalls I favor for casual wear (and wore daily at the NIH Clinical Center). (What can I say? I'm a country boy!) Anyhow, the pain got worse, and I decided it probably wasn't that either. Oddly, when it started, I had the prickly burning sensation on both sides of my chest. Later, it disappeared on the left, but my right shoulder blade area, and then my right shoulder, got involved. Cruising on the web led me to believe maybe the extraction of the PICC Line irritated a nerve or (horrors!) created some blood clots. Via email, NIH's Dr. Matt Olnes suggested another, more likely theory: shingles. According to Dr. Olnes, shingles sometimes "present" with this sort of sensation. I had chicken pox -- caused by herpes zoster, the virus that also causes shingles -- when I was a kid. Once you've got the virus, you get to keep it. It lives in nerve tissue and, in some folks, later in life, runs up those nerve fibers to cause a painful rash. It could be my lack of lymphocytes has created an opening for this to happen. So far, I've had no rash. And today the pain has nearly disappeared form my shoulder blade and shoulder, so now only my chest hurts. So, if Olnes' theory is correct, maybe the Valtrex is keeping the herpes zoster from becoming even more irritating. I'm going to hope so -- and hope for better counts next Tuesday.
__________________
Greg, 59, dx MDS RCMD Int-1 03/10, 8+ & Dup1(q21q31). NIH Campath 11/2010. Non-responder. Tiny telomeres. TERT mutation. Danazol at NIH 12/11. TX independent 7/12. Pancreatitis 4/15. 15% blasts 4/16. DX RAEB-2. Beginning Vidaza to prep for MUD STC. Check out my blog at www.greghankins.com |
|
#89
|
|||
|
|||
|
I'm sorry to hear it hasn't been smooth sailing, Greg. I'll be interested to hear if the shingles theory checks out -- my mother and sister both had shingles and their nerve pain definitely didn't come and go, it was pretty persistent from the get go. I'm hoping yours is a "friendlier" critter.
__________________
Catherine, wife of Bruce age 75; diagnosed 6/10/11 with macrocytic anemia, neutropenia and mild thrombocytopenia; BMB suggesting emerging MDS. Copper deficient. Currently receiving procrit and neuopogen injections weekly, B12 dermal cream and injections, Transfusions ~ 5 weeks. |
|
#90
|
|||
|
|||
|
Hi Greg-
I think it is way too early to be concerned about a small decrease in counts. Plus, different labs are always different. You cannot campare your local lab w/results you get from NIH. I have learned to only compare results from the same lab with each other; there is too much of a difference. Even here, locally, I used to get all my blood work done at the hema. office. Then, due to insurance, now I only get my CBC done there, but all else at the hospital lab sites and there labs are definitely different. So, I only compare numbers with the results from the same lab at this point. Hope you're other issue goes away!
__________________
Dx. 6/08 with AA, then changed shortly thereafter to MDS. Campath trial at NIH March '09 and have been transfussion independent since June '09 |
|
#91
|
|||
|
|||
|
Great news Greg! Keep us informed as to how it works! I'm happy for you. Blessings to you, Lori
__________________
Lori, female age 53 dx MDS-RAEB-II 15% blasts 10-2010. Induc Chemo 10/14/10 for 7 days - results unacceptable so 5 additional days chemo. Complete Remission 12/10/10!! SCT 1-11-11 remission achieved!!! BMB 1-29-11 100% Donor!  cgvh eyes,skin (Caringbridge.org/visit/loripatrick) cgvh eyes,skin (Caringbridge.org/visit/loripatrick)
|
|
#92
|
|||
|
|||
|
Thanks Catherine, Lisa, and Lori.
Catherine, Thanks for the report on shingles. I've known some folks who were afflicted, but not well enough to have followed their progress closely, so it's really interesting to hear what a "real " case is like. I will definitely be talking with Dr. Olnes about this Tuesday. I hope they might have even checked for herpes zoster counts (just out of curiousity). Lisa, What you say about labs is exactly what I have begun to expect. Plus, I know from my local doc that the local lab has had some problems getting their process calibrated correctly in the past. Have a great weekend! Greg
__________________
Greg, 59, dx MDS RCMD Int-1 03/10, 8+ & Dup1(q21q31). NIH Campath 11/2010. Non-responder. Tiny telomeres. TERT mutation. Danazol at NIH 12/11. TX independent 7/12. Pancreatitis 4/15. 15% blasts 4/16. DX RAEB-2. Beginning Vidaza to prep for MUD STC. Check out my blog at www.greghankins.com |
|
#93
|
|||
|
|||
|
Just a P.S. Greg -- Bruce is having bloodwork weekly right now, and there have been some dramatic variations from one week to the next up and down. The doctor can't explain it. I have started wondering about the accuracy of our "podunk" lab. We have started paying more attention to trends than the actual numbers, that keeps us from going too crazy.
__________________
Catherine, wife of Bruce age 75; diagnosed 6/10/11 with macrocytic anemia, neutropenia and mild thrombocytopenia; BMB suggesting emerging MDS. Copper deficient. Currently receiving procrit and neuopogen injections weekly, B12 dermal cream and injections, Transfusions ~ 5 weeks. |
|
#94
|
|||
|
|||
|
Hey Catherine!
Thanks for that. I'm thinking the same. In Bethesda now; NIH labs tomorrow. It should be interesting. I'll have a report later this week. Happy holidays! Greg
__________________
Greg, 59, dx MDS RCMD Int-1 03/10, 8+ & Dup1(q21q31). NIH Campath 11/2010. Non-responder. Tiny telomeres. TERT mutation. Danazol at NIH 12/11. TX independent 7/12. Pancreatitis 4/15. 15% blasts 4/16. DX RAEB-2. Beginning Vidaza to prep for MUD STC. Check out my blog at www.greghankins.com |
|
#95
|
|||
|
|||
|
Hi Greg,
Hope you get encouraging results from the NIH labs. Good luck & looking forward to your report later this week.
__________________
Lindy 56, low platelets, thrombocytopenia dx 2009, in watch & wait mode. |
|
#96
|
|||
|
|||
|
NIH Campath Trial Week 3 Follow-up
I've said a number of times on Marrowforums that one of the great ironies of MDS is that everything you do to make it better seems to first make it worse. A couple of weeks ago, I thought maybe I had dodged that bullet with the Campath trial.
But my labs at today (actually Tuesday) at NIH found my hemoglobin at 6.4 -- lower than it's been since diagnosis -- and we're only three weeks from my last transfusion. So I'm typing this on my laptop sitting in the Hematology Day Hospital on 3 South East South in NIH's Hatfield Building, getting two units of packed red blood cells. You may recall that, two weeks ago, I had some too-good to-be-true lab results that pegged my Hgb at 9.7, among other positive results, raising my expectations of rapid response. But Dr. Matt Olnes said he did not believe today's results represent a case of near-immediate response followed by near immediate relapse. Thus far, no patient in the trial has responded that way, while most have seen a weakening in their counts prior to response. The median time to response for the Campath trial is 96 days. Olnes felt that, instead, those earlier counts from my local lab were indeed too good to be true. So we are sucking down these RBCs and hoping for an early Spring. My platelets are holding steady at 60, which continues to be a relief. But my Neutrophils have taken a dive to 870, their lowest performance to date. If they dip to 500, I'll be taking Cipro and watching what I eat much more carefully. Hearkening back to my "War in my Bone Marrow" description of the sort of MDS that responds to immunosuppressive therapy [IST], we have now stopped the war that had my T-cells attacking my bone marrow stem cells. Now my marrow, kind of like Iraq, is trying to get itself organized, prop up a government, and get things running smoothly again. I just hope my marrow doesn't take as long as the Iraqis to get the job done. On a tragic note, Dr. Elaine Sloand, one of NIH's stalwarts on the MDS research front, died last week. Her husband died in early November. Though Dr. Olnes shared the news with me, he offered no details on cause of death. The staff was still visibly shaken by the loss of their colleague. It is a great loss for the community of MDS sufferers as well. Though Dr. Sloand wasn't as visible in webinars and patient conferences as some other MDS experts, the work she was spearheading in the lab and in the clinic was breaking important new ground in teasing apart the strands of the tangle that is MDS. Dr. Olnes said he and his colleagues planned to honor her memory by continuing her work. I wish them Godspeed in that effort. He also reported that the NIH Campath trial for MDS has been extended from the original complement of 43 patients to a total of 78, so more folks who feel IST might be the way to go in treating their MDS will have the opportunity to try this alternative to ATG.
__________________
Greg, 59, dx MDS RCMD Int-1 03/10, 8+ & Dup1(q21q31). NIH Campath 11/2010. Non-responder. Tiny telomeres. TERT mutation. Danazol at NIH 12/11. TX independent 7/12. Pancreatitis 4/15. 15% blasts 4/16. DX RAEB-2. Beginning Vidaza to prep for MUD STC. Check out my blog at www.greghankins.com |
|
#97
|
|||
|
|||
|
Greg-
I am shocked to read about Dr. Sloand. She was the PI when I did the trial back in 09 and Matt Olnes, at the time, was the attending. I knew when their roles switched that her husband had been very ill and that was the likely reason for the change. That is really sad. I know she was extremely focused in her work. We are fortunate, however, that Dr. Matt Olnes is also exceptional! I know we are in excellent hands with him as the PI. One thing I will say to you, PATIENCE!! You need to have it. Your counts will go up and down for a little while yet. It took me 6 months to really see the success of Campath. Don't get discouraged! Thanks for the news. Good and bad........... A sad loss to the NIH.
__________________
Dx. 6/08 with AA, then changed shortly thereafter to MDS. Campath trial at NIH March '09 and have been transfussion independent since June '09 |
|
#98
|
|||
|
|||
|
Lisa,
Thanks for the encouragement. I'm not really expecting to have a faster than average reaction to Campath -- and Dr. Olnes made it pretty clear that everyone seems to react a bit differently. It's great to have someone who has already been through this to compare notes with. I was really bummed to hear about Dr. Sloand. Though I never had the pleasure of meeting her, I've read so many of her articles. And I really respect the way she combined the lab and clinical work to really nail down how the whole immunosuppressant angle worked. It's a great loss to all of us. Happy Holidays! Greg
__________________
Greg, 59, dx MDS RCMD Int-1 03/10, 8+ & Dup1(q21q31). NIH Campath 11/2010. Non-responder. Tiny telomeres. TERT mutation. Danazol at NIH 12/11. TX independent 7/12. Pancreatitis 4/15. 15% blasts 4/16. DX RAEB-2. Beginning Vidaza to prep for MUD STC. Check out my blog at www.greghankins.com |
|
#99
|
|||
|
|||
|
Greg --
This disease guarantees us all a wild emotional roller coaster ride, doesn't it? One of the things Dr. Paquette (the MDS Specialist at UCLA) said to us in October was "Patience is key." Easier in concept than practice. I'm hoping the pain in your upper body has improved. Also...off topic a bit -- Bruce met with our MD yesterday (a very talented former biochemist and now functional medicine guy) about the copper issue. The hematologists with whom we've discussed Bruce's low copper levels weren't too concerned about it being in the 60's because it "wasn't that low." The family doc believes that it is still WAY low -- that to really help in getting the bone marrow going, it needs to be at the middle, not the bottom, of the range. So he upped Bruce's copper supplementation.
__________________
Catherine, wife of Bruce age 75; diagnosed 6/10/11 with macrocytic anemia, neutropenia and mild thrombocytopenia; BMB suggesting emerging MDS. Copper deficient. Currently receiving procrit and neuopogen injections weekly, B12 dermal cream and injections, Transfusions ~ 5 weeks. |
|
#100
|
|||
|
|||
|
NIH Campath Trial Follow-Up Addendum - Shingles
Hey Catherine!
Thanks for reminding me about the upper body pain. I had forgotten to provide follow-up on that. A few days before my one-month follow-up trip to NIH, the burning, tingling pain that I had been experiencing in my right chest, shoulder, and shoulder blade began to gradually fade away. By the Tuesday of my appointment, it was more the memory of a pain than actually pain, and now three days later, even the memory is faded. The verdict: it wasn't shingles. Dr. Olnes confirmed what Catherine described as her experience with her mother and sister: once you get the herpes zoster virus stirred up, it doesn't let up until it has coursed its way up your nerve fibers, infested the lymph near your skin, and broken out into a painful rash. So, the Campath didn't provoke a shingles outbreak in me. What did cause the pain. I'll likely never know. I did travel back from NIH sleeping in the back of a smallish Jeep, wearing my signature bibbed overalls. Maybe my awkward position pulled on the straps enough to compress a peripheral nerve and create the numbness and pain. In any case, I'd rather have a mystery than shingles. Happy Holidays! Greg
__________________
Greg, 59, dx MDS RCMD Int-1 03/10, 8+ & Dup1(q21q31). NIH Campath 11/2010. Non-responder. Tiny telomeres. TERT mutation. Danazol at NIH 12/11. TX independent 7/12. Pancreatitis 4/15. 15% blasts 4/16. DX RAEB-2. Beginning Vidaza to prep for MUD STC. Check out my blog at www.greghankins.com |
 |
| Thread Tools | Search this Thread |
|
|
 Similar Threads
Similar Threads
|
||||
| Thread | Thread Starter | Forum | Replies | Last Post |
| Pilot study of Alemtuzumab (Campath) at NIH | Barbara2007 | Clinical Trials | 9 | Thu May 5, 2022 12:38 AM |
| New Promacta (Eltrombopag) Clinical Trial at NIH | Sally C | Clinical Trials | 73 | Sun Dec 30, 2018 05:52 AM |
| NIH Trial - Plt Count Level Feedback/Experience | disco3md | AA | 1 | Wed Jun 28, 2017 01:08 PM |
| NIH Trial (Eltrombopag & Cyclosporine) | disco3md | Clinical Trials | 0 | Mon Jun 26, 2017 05:02 PM |
| Subcutaneous Campath Trial | Nadia T | Clinical Trials | 3 | Fri Dec 20, 2013 09:06 PM |