
| Home Forums |
|
|||||||
| Transplants Bone marrow and stem cell transplantation |
 |
|
|
Thread Tools | Search this Thread |
|
#1
|
|||
|
|||
|
Can Drugs/Transfusions interfer with BMT success?
I am new to Marrowforums. I am a 50 year old female, and I was diagnosed May 2011 with Hypoplastic MDS with an IPSS score of 1. Cytogenetics showed 2 abnormalities on chromosome 15, blasts less than 5%,and all 3 blood counts are low. Currently at a watch and wait status. On the registry for a MUD with a potential transplant at Princess Margaret in Toronto.
Other than fatigue and slight shortness of breath I am living a normal life. My first referral was to a team of doctors in London, Ontario and their first suggestion was a BMT because I was young and strong and it is the only cure. The specialist in MDS, at Princess Margaret suggested drugs and transfusions would be the next course of action. My question deals with the timing of things. . . . since I am young and strong I don't want to delay the BMT, but on the other hand it has serious risks! If I use some of the drugs and transfusions does it interfer with a successful BMT, and with the delay I become a bit weaker? Currently my counts aren't quite low enough to need treatment, and there isn't a match found yet. I am just wondering what is the ideal pathway to follow for the greatest chance of success.  |
|
#2
|
|||
|
|||
|
drugs and treatments with future BMT
If you look for squirrelypoo's postings (mellisa) you will see that she is at least one person who had treatment for AA and then has gone on to have a BMT and is doing really well.
At 51 I was told I was too old for a BMT and they would do this as a last resort as my sibling was not a match. However, saying that, there is a gentleman on here who is older, and had an unrelated donor and is doing very well...its luck of the draw really and on how healthy you are to begin with. Sit tight, someone else with far more knowledge will be able to answer you more fully tho. x |
|
#3
|
|||
|
|||
|
A much-too-long non-answer to your very excellent question
Janice,
You have asked the $250,000 question. This is an area of hot debate amongst the experts -- and patients. And, ultimately, it all comes down to a matter of your own tolerance for risk and for living with a disease. Transplanters will tell you that your best chance for a successful transplant is to do it as quickly as you can. And they will be right. You take a strong 50-year-old with relatively mild symptoms, a low blast count, low transfusion requirements and you transplant them. Or you take a 60-year-old whose MDS has just converted to AML, put them through a few courses of Vidaza to try to get rid of the chromosomal irregularities and you transplant them. You can probably guess which patient is going to have the best chance of success, get through transplant with the fewest problems, and have the least chance of dying in the transplant process. But, on the other hand, that 50-year-old may be doing just fine. So why does she want to take a one in three, or one in four, or one in five chance that she'll be one of the folks who gets labeled "transplant-related mortality." Why does she want to take a year out of her life to go through a life-threatening and life-altering process? Why does she want to risk getting seriously bad GVHD and taking lots of meds for the next ten years that will make her feel worse than she feels right now? Someone would decide to do that because they want to be cured. Some folks simply cannot live with the knowledge that they harbor within their bone marrow a deadly disease that, a year from now, six months from now, or a week from now, could explode into something truly terrifying. Others will do that because they have a strong positive outlook, have read the transplant success stories of folks on marrowforums or elsewhere, and they feel lucky, or confident, or blessed. There's a ton of research out there on transplant, but there's not a lot that can really answer your question. One study that tried, and many MDS doctors will refer to, is a big, complicated, statistical study led by Dr. Corey Cutler at Harvard. He looked at a bunch of MDS patients who were transplanted, and did some sophisticated statistical analysis to figure out life expectancy for folks transplanted right away, two years out, or at the point they progressed to AML. Low-risk patients transplanted at progression lived and average of 7.21 years; those transplanted at diagnosis, 6.51 years. For INT-1 folks, like you and me, transplanted at progression, life expectancy was 5.16 years, versus 4.61 years if transplanted at time of diagnosis. So lower risk folks might want to delay transplant. On the other side of the coin, INT-2 and high risk folks lived longer if transplanted right away. If you're like me, you look at those numbers and think: Heck! I plan to live a lot longer than any of that! Plus, the data that those numbers is based on was all collected before Revlimid, Vidaza, or Dacogen were approved (in the US, at least.) And the transplanters are improving their procedures, and their numbers. In other words, that's all pretty interesting, but it doesn't do much toward helping an individual decide what to do. That's enough from me for now. I hope it's somewhat useful, and I'm sure others more knowledgeable will chime in. Two other thoughts: I strongly recommend you watch a lot of webinars and presentations done by transplanters. In particular, go watch to this page and watch the one by Matt Kalaycio, MD, FACP. He's very matter of fact about the risks, which can be rare in a transplanter. Second, I can't put my browser on the link right now, but I saw a presentation by Bart Scott, another well-known transplanter from up in Seattle. He said that, if he were diagnosed, he'd want a transplant right away, ASAP. "But I've learned to learn from my patients," he said, and then related the story of a 50-year-old guy, diagnosed with MDS, who wouldn't go for transplant right away, because the most important thing in his life was his daughter's upcoming bat mitzvah, about a year in the future. That's the way I see it: you have to listen to everyone's story, listen to all the experts, listen to know-it-alls like me, really understand the risks, really understand the potential benefits, lay down your money, and make your choice. Good luck! Greg
__________________
Greg, 59, dx MDS RCMD Int-1 03/10, 8+ & Dup1(q21q31). NIH Campath 11/2010. Non-responder. Tiny telomeres. TERT mutation. Danazol at NIH 12/11. TX independent 7/12. Pancreatitis 4/15. 15% blasts 4/16. DX RAEB-2. Beginning Vidaza to prep for MUD STC. Check out my blog at www.greghankins.com |
|
#4
|
|||
|
|||
|
How to Decide. . . Now or Later!!!
Thanks Greg,
I really appreciate you addressing my question. The hospital in London, Ontario said transplant ASAP since I was young and strong. The center for MDS Excellence at Princess Margaret said wait and watch, then drugs and transfusions, then transplant. The only long term cure is transfusion, so , in my opinion, I don't want any previous treatment to stand in the way of a cure! Currently I am not needing any treatment. A MUD has not yet been found so if I were to need a treatment, I would have little choice but to accept it. My hope is that a BMT would occur before other treatments are necessary. BUT. . . edvancements in medicine occur which may result in the risky BMT not being required. SO, my thought is to hopefully make the right decision when my need for a treatment arises. My gut says to go for the BMT since I am younger and strong. I was recently running 3times a week and weight training, and playing golf along with working full time; which suggests I have strength on my side. I guess some of the decision will be determined by the match to my donor. A perfect match will make my decision for the transplant much easier! Thank you for your input. Please stay in touch! All the Best, Janice 
__________________
Female, age 52 - Diagnosed May, 2011 Hypoplastic MDS. Cytogenetics showing 2 abnormalities on chromosome 15. Blasts<5%, IPSS of 1. All blood counts low, but no treatment; watch and wait. Registered for MUD; on Feb. 23/12 two donor matches found but returned since not needed yet! |
|
#5
|
|||
|
|||
|
Quote:
Just to clarify for others, you meant the only long term cure is a transplant. You clearly see the tradeoffs, which Greg explained so well. Like my wife, you want to be cured and don't want to wait too long. My wife had fewer choices at the time (before MDS drugs were available) but she was confident about the decision to go to transplant. Your donor match is certainly an important factor that's yet to be determined. I'm glad you are otherwise healthy and active. That will serve you well. |
|
#6
|
|||
|
|||
|
And another thing . . . .
Hey Janice!
Sounds like your folks at Princess Margaret have read the Corey Cutler study. I forgot to mention that not only was the data from that study collected prior to the approval of the new MDS drugs, but it also included only myeloablative transplants (the big ones, no reduced intensity transplants) and only transplants with HLA-identical sibling donors. In other words, the world has changed pretty completely since then. Folks who are wary of transplant have a lot more options and folks who want a transplant have a lot more options, too. But the study was useful in that it threw up a read flag and said "Whoa! Just because a disease is nasty and this dangerous procedure is the only "cure," that doesn't make it right for everyone." And maybe because it was from Harvard, or maybe because Cutler wrote it, or maybe because the statistics were way over the head of most docs who read it (me too!), it got some attention. It's great that you aren't terribly symptomatic and have some time to decide what to do. There are lots of great transplant journals on marrowforums. Definitely read about Melissa's experience, check out Laura's recent difficulties, and read Karen's blog for a "just had it" peek at the experience of a 50-something MDS patient. There are lots of others, all very useful. Take care! Greg
__________________
Greg, 59, dx MDS RCMD Int-1 03/10, 8+ & Dup1(q21q31). NIH Campath 11/2010. Non-responder. Tiny telomeres. TERT mutation. Danazol at NIH 12/11. TX independent 7/12. Pancreatitis 4/15. 15% blasts 4/16. DX RAEB-2. Beginning Vidaza to prep for MUD STC. Check out my blog at www.greghankins.com |
|
#7
|
|||
|
|||
|
Hi Greg and Neil,
I met we a leading MDS doctor at Princess Margaret. Her thoughts, I believe, are that both courses of actions have risks(drugs & transfusions vs. BMT). Although the previous hospital suggested BMT immediately, she was hoping to buy some time since there are new drugs constantly being tested etc. If I were to remain free of treatment for a period of time, even more medical advances are possible! On the transplant side, she suggested that the mini transplant is certainly a good option. If a perfect marrow match is found that would certainly be a compelling factor for the transplant. By the way, for all those needing a transplant, I am happy to say, that I have been fortunate to have numerous people join the registry in a willingness to help. By nature I am a planner. . . personally, at work and for social situations. I already have next week's menu for after golf planned! I find it hard not to be able to know what is coming next and within what time frame, with this disease. I want to plan the best route for when I need treatment. Path A drugs and transfusions or Path B a transplant. Although as I read and learn more, I believe I can go down Path A for a while and then switch to Path B??? I just don't want to go too far down Path A if it interfers with the success of Path B (BMT). Thanks for the links to some of the other people's journey. Neil, I have read your wife's journey when I first found this site. A very touching and inspiring story. Upon reading it, I felt that my disease would perhaps take a similar path. I have read some of the others, but I will be sure to read all of them. Oh, one other question. I am a teacher, if I need drugs and transfusions, at that time will I still be able to work? Any idea? Thanks for all your insight. Janice 
__________________
Female, age 52 - Diagnosed May, 2011 Hypoplastic MDS. Cytogenetics showing 2 abnormalities on chromosome 15. Blasts<5%, IPSS of 1. All blood counts low, but no treatment; watch and wait. Registered for MUD; on Feb. 23/12 two donor matches found but returned since not needed yet! |
|
#8
|
|||
|
|||
|
Now, to get down to business, and go out on a limb . . .
Janice,
My initial response to you got way off into the general philosophy of transplant and didn't really answer your more practical question. So I'll take a stab at that. Transfusions - Having RBC transfusions shouldn't really interfere in any way with your ability to work or play. The typical practice at my hospital is to transfuse two units of packed red blood cells at a go. Each unit takes two hours. When you figure the time to get registered, set up, etc. it winds up being most of the day in the hospital or day surgery unit or treatment room. Unless you have some sort of reaction to the blood (very rare), you can go from the hospital straight to work. The issue that usually confronts folks is frequency -- how often they have to get a day off from work because they need a transfusion. Transfusion and transplant - This is a can of worms. I think there's data out there indicating folks with a lot of transfusions don't do as well with transplant. And I know there's data out there that says folks with very high ferritin counts (which tends to go up with every transfusion) don't do as well with transplant. My doc at the National Institutes of Health says you have to take all this with a grain of salt. It's all based on after-the-fact analysis and, in that situation, you don't know what other factors might be coming into play. Maybe the folks with a lot of transfusions were just generally in worse shape. So, you will find some transplant centers that will give you Exjade or some other drug to bring your ferritin down before transplanting. They don't do that in the transplant unit at NIH. As my doc said, "There not a lot of good data on this, so people have a lot of strongly held opinions." Vidaza & Dacogen - All three of the major MDS drugs, Revlimid, Vidaza, and Dacogen, are unfriendly to your bone marrow. In other words, they are almost guaranteed to make you sicker before they make you better. Vidaza and Dacogen are similar: you have to go into the doctors office or treatment center for 5-7 days in a row once month Some people do okay during the treatment and right afterwards; some people feel like crap; almost everyone sees their counts go down. Doesn't sound all that work-friendly, at least during treatment week, to me, but I don't have any personal experience with this. You can search for "Vidaza" in the threads and get a good idea of the range of experience. The studies that got these drugs approved were with high-risk patients. There's no good data that I have seen that justifies giving Vidaza or Dacogen to low-risk or INT-1 patients. Some centers use it as a bridge to transplant: you're high-risk, have a lot of messed up chromosomes, and they want you to take it to try to suppress those bad clones before starting the transplant process. So, taking these drugs isn't going to hurt your chances for a successful transplant. But, if you're on them, it's probably because your disease is progressing. Revlimid -- Revlimid is approved in the US for folks with deletion 5q, but there are on-going clinical trials of it in low-risk, red cell transfusion dependent patients. It tends to lower platelets pretty significantly, so is a less happy choice for low-risk folks who mainly have platelet problems. Aside from the platelet issue, my doc (who has a lot of experience using it in multiple myeloma patients) says it is "very well tolerated." It's a pill, so you can take it at home. Unless you had an allergy to it, I wouldn't see it interfering with work or reducing your chances for a successful transplant. IST - Immunosuppressive therapy -- the ATG plus cyclosporine that a lot of AA folks wind up doing -- is a possible treatment for lower-risk MDS. In fact, folks with hypocellular marrow are one of the groups that have a higher probability of success with IST. I did a clinical trial with another IST agent called Campath. The ATG part of the treatment is going to put you in the hospital for several days (I'm not sure exactly how many). The cyclosporine is a pill you take afterwards. It has some pretty nasty side effects and there's a whole complex deal with trying to slowly, slowly wean you off of it. I haven't had it myself, so I can't relate how it relates to work and play, but you can search marrowforums for "cyclosprine" and get a ton of info. IST should interfere with transplant, according to most folks. My transplant doc, who uses ATG in the transplant process, didn't want me to use it prior to transplant. That was one of the reasons I went for Campath instead. Looking ahead -- You don't even need transfusions now, so you are in the catbird seat. If you eventually need RBC or Platelet transfusions, which one you need may tell you which drug therapy makes the most sense -- and whether your disease is progressing. All in all, I don't think any of the drug therapies are, in themselves, likely to make a transplant less successful. Whether a few years of monthly transfusions will complicate transplant seems to be a matter of significant disagreement among the experts. (If any of you other MDSers out there think what I have just written is bunk, I do hope you will jump in and set me -- and Janice -- straight.) Good luck! Greg
__________________
Greg, 59, dx MDS RCMD Int-1 03/10, 8+ & Dup1(q21q31). NIH Campath 11/2010. Non-responder. Tiny telomeres. TERT mutation. Danazol at NIH 12/11. TX independent 7/12. Pancreatitis 4/15. 15% blasts 4/16. DX RAEB-2. Beginning Vidaza to prep for MUD STC. Check out my blog at www.greghankins.com |
|
#9
|
|||
|
|||
|
Greg,
Thanks for giving me what you know about treatments, in such an easy to follow manner! I have been reading and listening to archived webinars to try and get the information you have given me in such a concise and logically organized manner. Your help is greatly appreciated. From what you have outlined then, it appears as though I would continue on the "wait and watch" until my counts suggest the need for drug therapies and transfusions. At that point, I would have to see how the treatments are effecting me and the time needed for them, regarding continuing to work. ( I have 4 years to go to achieve an unreduced retirement pension). Hopefully also at that time, a MUD has been found and I am assuming I would move towards a BMT, with the previous treatments not interferring with the success of the BMT. My last counts were: WBC 2.8, Hemoglobin 11.4, platelets 40, MCV 102 and Netrophils were .54. Are you pursuing a BMT? If so, at what point is it recommended? Thanks for all your helpful information, Janice
__________________
Female, age 52 - Diagnosed May, 2011 Hypoplastic MDS. Cytogenetics showing 2 abnormalities on chromosome 15. Blasts<5%, IPSS of 1. All blood counts low, but no treatment; watch and wait. Registered for MUD; on Feb. 23/12 two donor matches found but returned since not needed yet! |
|
#10
|
|||
|
|||
|
Greg has given some great information and a fantastic analysis. Two thumbs up there!
I just want to address one other aspect and possibly get some feedback from some of the others. We've all heard repeatedly that BMT is the only cure, and this weighs heavily in most of our thinking when making a decision. Lately, however, I keep hearing from people who have relapsed after transplant, and even some of the doctors in the AA&MDSIF's videos refer to relapses post-BMT, and also say that there is no significant difference in the survival statistics between BMT and IST (where that is an option). So for me, that puts the "cure" aspect in a somewhat different light. If relapse is a possibility in both scenarios, and so is durable remission, then it's not so clear cut. I realize that everybody is likely to be somewhat biased in favor of whatever course of treatment they have chosen, and that is the probably the best thing for maintaining a positive mental state. I'm not trying to change anyone's mind about their treatment decisions, but I'm just wondering how many people would still choose to go with the increased risks, expenses and long recovery time of a BMT if they weren't seeing it as a choice between "cure" and "no cure"? Obviously a lot would depend on the prognosis, the quality of the available match and what the other options were. Speaking only for myself, I've followed enough cases of debilitating GVHD and other complications/side effects that it has become increasingly difficult for me to look at the process as anything but a last resort.
__________________
-Lisa, husband Ken age 60 dx SAA 7/04, dx hypo MDS 1/06 w/finding of trisomy 8; 2 ATGs, partial remission, still using cyclosporine |
|
#11
|
|||
|
|||
|
Hey Janice!
I just hope I'm not leading you astray here . . . I'm sure if others have contrasting data to add, they will jump in. I think what you suggest makes a lot of sense. In fact, when I was first diagnosed, my local doc initially wanted to put me on Vidaza. But I did the research and found out it really didn't make sense. So we adopted a watch-and-wait posture, while consulting with a transplant center, until I found out about IST and the Campath clinical trial at NIH. Because of the theory behind the use of IST for MDS, it made sense for me to dive into that, before my T-cells created any more havoc in my marrow. (You can read about that whole concept here.) Otherwise, I would have stuck with watch and wait, even though I was having transfusions every six weeks. Through consulting with the transplant center, I discovered that I have no sibling donor options, but have at least three solid matches in the registry. Knowing that is sorting of like having an ace in the hole; it gives one a bit of comfort about waiting a while for transplant. Though my very aggressive fireball transplant doc would have me in the transplant ward tomorrow if I'd let her, I'm waiting until I see clear signs of disease progression. This is a very personal decision for everyone, so I am in no way suggesting that my line of thinking is the only correct way of thinking -- heck, it might be just plain dumb. Risk - You can read all kinds of statistics about transplant, but the overall impression I walk away with is this: there's about a 50 percent chance that either A. the transplant will kill you, or B. You'll get some really nasty GVHD that's worse than monthly transfusions, or C. You'll relapse in two years. There's maybe a 25% chance that you come away with only minor GVHD that's about as annoying as a transfusion every month. And there's maybe a 25% chance that you come out with utterly no problem, better than you were before. Do not try to take any of those percentages to the bank. It is just my overall impression from watching all those videos and reading a ton of stuff. Until my transfusion requirement becomes unbearable, or my platelets or neutrophils decline into the danger zone, or I get a bunch of blasts or some nasty chromosomes, I'm probably not going to have a transplant, just based on the odds as I see them. But, you can improve your odds. The things that really hurt your odds in transplant are being older, in poor physical condition, or having other diseases (co-morbidities). So, figuring at some point I might need a transplant, I have lost 30 lbs, exercise more, and eat better than I used to. You sound like you have it all covered in that department. Life - I'm 54. I run a small community newspaper -- a real Mom and Pop where there's no way the operation as currently configured can run without Pop. I depend on that business for my health insurance, as well as my income. So I'm not in a good position to take a year off (or even six months off) to have a transplant. Knowing that I might have to have a transplant at some point, I am carefully working to bring other folks into the operation and training them to cover bits and pieces of my job, while trying to expand the business to pay for them, and getting it in a position where, if worse came to worse, I could try to sell it. That's where I'm at in my decision-making. My disease is in a bit of a transition mode right now. You can read more about where I've been and where I am on my blog (link below). Sometimes you folks north of the border use blood count units that aren't exactly the same as the ones customarily used down here, so I'm not sure whether I know what I'm looking at with your counts. If the units are the same as ours, your platelets are getting on down there and your neutrophils are at about the level that my docs at NIH would have you on Ciprofloxacin to prevent infection. Can you post the reference ranges on those counts? It could be just that we are using different units. From my perspective, I always feel lucky that it's mostly my reds that give me trouble. Sure, that makes me tired, but MDSers get into real problems when they have bleeding caused by low platelets and infections from a low neutrophil or lymphocyte count. Sorry to blather on, but responding to your questions is actually helping me put some stuff down that's been running around in my brain. Take care! Greg
__________________
Greg, 59, dx MDS RCMD Int-1 03/10, 8+ & Dup1(q21q31). NIH Campath 11/2010. Non-responder. Tiny telomeres. TERT mutation. Danazol at NIH 12/11. TX independent 7/12. Pancreatitis 4/15. 15% blasts 4/16. DX RAEB-2. Beginning Vidaza to prep for MUD STC. Check out my blog at www.greghankins.com |
|
#12
|
|||
|
|||
|
Greg,
I greatly appreciate the information and thoughts going back and forth. I am new to this disease so your information and Lisa's comments greatly help. I can see Greg why you have the BMT on the back burner with your job situation, but at lease you do have your ace in the hole when needed! My one sibling and 2 daughters are not a match so they are currently looking. I hear it may take 6 months to determine if there is match. And, yes in the meantime, I appear to be doing fine. In June 2008 it was determined my platelets were low and we were monitoring that. Other than bruising, I have had no difficulty. In my opinion I have always bruised easily. I never, ever get sick. Go figure that with the lower WBC count. I think what I have just does a darn good job. My Hemoglobin is not that low, but I do feel a bit fatigued and some minor shortness of breath. But. . . . up until May I was running 5K or 3 miles at least 3x a week. I am still golfing, going out shortly, and I walk all 18 holes. So it isn't bothering me much! With being fit, young for this disease, and my first specialist saying you are a perfect candidate for a BMT, since that is the only cure, my thoughts only went in that direction. However, I have also done a lot of reading, and now speaking with others and the BMT has started to show a great deal of risk, both during and afterwards. The last specialist, Dr. Karen Yee was also suggesting there are great advances in the medications so if that point for me is down the road in time, there may be more options, other than the BMT. When I first started reading, it appeared as though people that were older were having the treatments and those few that were younger having the BMT. That made sense due to the gruelling process of the BMT, unless someone was at a point of no choice. I greatly appreciate the information and prospective that you have given me regarding other options, and how the use of treatments may not interfer with the BMT if needed. Greg, I will get back to you tonight with the Canadian ranges for the blood counts. Sorry, got to go. Thanks for all your input. If others have anything to add I would appreciate it as well. Greatfully, Janice
__________________
Female, age 52 - Diagnosed May, 2011 Hypoplastic MDS. Cytogenetics showing 2 abnormalities on chromosome 15. Blasts<5%, IPSS of 1. All blood counts low, but no treatment; watch and wait. Registered for MUD; on Feb. 23/12 two donor matches found but returned since not needed yet! |
|
#13
|
|||
|
|||
|
Quote:
I'm glad you brought this up. I noted up front that it's kind of a controversial subject, because it's important to be 150% behind whatever decision you finally make. And STC is a real miracle for some people -- often people who really and truly have no other viable option. But, when you're making a decision, it's also important to look at all sides of the issue -- and to understand that transplanting a 15-year-old with AA is very, very different than transplanting a 50-something with high-risk MDS. That's why I really really like the Matt Kalaycio presentation, because he's a transplanter, but he's very, very clear about how risky an option that is. He also talks about STC as "potentially curative," which is a better formulation than saying it's "the only cure for MDS." Here's a famous graph that you've probably seen in the presentations or the literature: 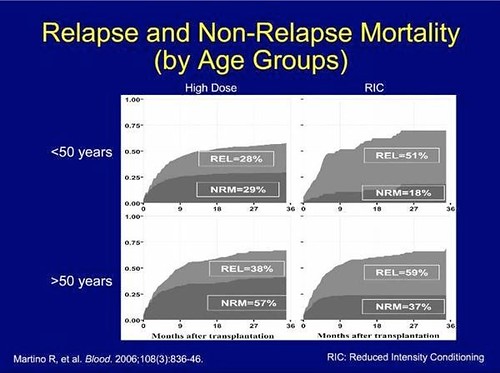 13.SCT Comparison Study by hankins.greg, on Flickr So, what does it say? It's comparing "big" myeloablative transplants (on the left) with a reduced intensity "mini" transplant. REL is relapse and NRM is "Non-Relapse Mortality" So, the graph shows that, after three years, amongst folks under 50 years of age, three years out, there's a 29% chance the transplant will have killed the patient, and a 28% chance they will have relapsed. Among older folks, there's a 57% chance the transplant will kill you and a 38% chance you'll relapse. If you look at "mini" transplants among older folks, the percentages are reversed -- less death, more relapse. Now, all the usual caveats apply. The study was done in 2006, the data is from 1998-2001. Presumably, transplanters have gotten better in the intervening years. There were all sorts of folks in the sample from really high risk to relatively low-risk. If you're a really healthy 50-something hot dog, you're likely to do a lot better and not be in either the dead or the relapsed category. Still, amongst the 171 patients over 50 in this sample who had a standard ablative transplant, there was a nearly six in ten chance they'd be dead in ten years -- and a nearly four in ten chance they'd relapse. These are scary numbers for a therapy that's supposed to be a "cure." If you go and spend a week reading The Emperor of All Maladies (which I reviewed here), you'll learn a bit about how "cure" became the key word in cancer research, and how that may have been more about politics and marketing than about medicine. Many, many, many folks really, really need a transplant. It is truly the very best option for many people. I fully expect that I will have one, and I admire and value the wonderful folks who have shared the good, the bad, and the ugly of their transplant experience on these forums, so we all can learn. But, when I hear that a doctor has advised transplant for a patient with no clinically significant symptoms, no transfusion requirements, and excellent quality of life, it pretty much curls my hair, after which steam starts shooting out of my ears. I understand that some folks, like Dr. Bart Scott himself, have to be cured at all costs. But, from my perspective as a patient trying hard to be educated about my options, it's not really responsible medicine to lead folks down that road without first being really honest about what they are getting into. Take care! Greg
__________________
Greg, 59, dx MDS RCMD Int-1 03/10, 8+ & Dup1(q21q31). NIH Campath 11/2010. Non-responder. Tiny telomeres. TERT mutation. Danazol at NIH 12/11. TX independent 7/12. Pancreatitis 4/15. 15% blasts 4/16. DX RAEB-2. Beginning Vidaza to prep for MUD STC. Check out my blog at www.greghankins.com |
|
#14
|
|||
|
|||
|
Quote:
And thanks for the link to Dr. Kalaycio's talk. That was one I hadn't watched yet, and it was excellent. He really lays it all on the table, and I hope that anyone who is considering a transplant will take the time to watch it. He actually had a chart of the criteria he uses to determine at what point someone becomes a suitable candidate for SCT. I think that may help answer some of your questions too, Janice.
__________________
-Lisa, husband Ken age 60 dx SAA 7/04, dx hypo MDS 1/06 w/finding of trisomy 8; 2 ATGs, partial remission, still using cyclosporine |
|
#15
|
|||
|
|||
|
Greg,
You are right. The word "cure" is misleading. BMT is a cure if you don't die during the process or afterwards due to GVHD or an Infection. Greg were you referring to me being recommended for a transplant, without symptoms yet? In case you were, the team in London, Ontario were suggesting to ultimately have a BMT but they weren't suggesting it until further down the road when there were at least symptoms and choices of a pathway needed to be taken. That is one of the reasons I was asking about A) does any of the treatments interfer with the success of the BMT and B) the timing of the transplant because as a fit, relatively younger, patient waits for the BMT, are they now at an increased risk. . . so when is the "tipping point" as I call it? Greg, here are the Canadian Normal Blood value ranges: (from Dr. K. Yee) Hb over 120 or in the US over 12.0 (11.6) Plt 150-400 (40); WBC 4 -11 (2.8) ; Neutrophil 2 -7 (.54) (mine) Again, thanks for the excellent discussion. Through our discussion I realized that partially the reason you have not proceeded to a BMT now is due to work and health care benefits. Sometimes in reading people's situation, I have wondered why they had choosen a particular pathway with their disease, but without all the circumstances the reason behind the choice is never clear. This has been enoromously helpful, and I am extremely grateful. I return to London Hospital on Sept. 21 so this gives me much more information to discuss! Thanks again, Janice 
__________________
Female, age 52 - Diagnosed May, 2011 Hypoplastic MDS. Cytogenetics showing 2 abnormalities on chromosome 15. Blasts<5%, IPSS of 1. All blood counts low, but no treatment; watch and wait. Registered for MUD; on Feb. 23/12 two donor matches found but returned since not needed yet! |
|
#16
|
|||
|
|||
|
Hey Janice!
Sorry . . . my intent wasn't to slander your docs, I was thinking not of your specific case so much as the general state of things. Docs are all different (like people) -- some more anxious to get moving on a therapy; some more apt to move with a degree of caution. We're kind of culturally programmed (at least in the US) to want a cure, right now, and sometimes docs get infected with that mania. Your ranges are pretty much the same as the ones I'm used to -- so it looks like you may have more of a WBC and Platelet problem than an RBC problem. It's great that they haven't caused you much trouble. I participated in a conference call on MDS with Dr. Yee; she was great! Very knowledgeable and able to talk about MDS in language a layperson could understand. Work and insurance are indeed big factors in my decision-making about transplant right now. But, frankly, even if I were a billionaire, I wouldn't do transplant at this stage in my disease. The risk profile just doesn't cut it for me. And, when I say risk profile, I'm not just thinking about risk of death. I'm instead thinking about the quality of life issues -- that is, coming out sicker on a day-to-day basis than you went in. But, for some folks, the strain of knowing you are living with an incurable disease that can get nasty fast -- that is a quality of life issue. Everyone's different in terms of what makes sense for them. Most folks who have transplants don't have much of a choice; the disease forces your hand at some point. I fully expect to get there. But getting there while I'm still a lower risk MDS-er doesn't make sense from where I am sitting. Take care -- and have a great weekend! Greg
__________________
Greg, 59, dx MDS RCMD Int-1 03/10, 8+ & Dup1(q21q31). NIH Campath 11/2010. Non-responder. Tiny telomeres. TERT mutation. Danazol at NIH 12/11. TX independent 7/12. Pancreatitis 4/15. 15% blasts 4/16. DX RAEB-2. Beginning Vidaza to prep for MUD STC. Check out my blog at www.greghankins.com |
|
#17
|
|||
|
|||
|
Sekeres - To treat or not to Treat
Hi all!
Just got an email from AAMDS, which I'm sure most of you all got as well, about a September 1 webinar by Dr. Mikkael Sekeres called "To Treat or Not to Treat: Making Treatment Decisions in MDS." Here's the link to the sign-up page. Very timely, given what we've been talking about in this thread. And Sekeres is always good to hear. The Q&A with him, if the questions are good ones, can be particularly enlightening. So you all sign up and ask some good questions! Take care! Greg
__________________
Greg, 59, dx MDS RCMD Int-1 03/10, 8+ & Dup1(q21q31). NIH Campath 11/2010. Non-responder. Tiny telomeres. TERT mutation. Danazol at NIH 12/11. TX independent 7/12. Pancreatitis 4/15. 15% blasts 4/16. DX RAEB-2. Beginning Vidaza to prep for MUD STC. Check out my blog at www.greghankins.com |
|
#18
|
|||
|
|||
|
Quote:
As for part A, on that same video there is a Q&A session with both Drs. Kalaycio and Maciejewski. Dr. M also had a chart, this one showing the effect of prior treatment on BMT. To summarize, those who respond to medication are actually in a better position to undergo a transplant than they would have been without treatment. On the other hand, those who don't respond tend to do worse than they would have done without the drugs. So it's another Catch-22. There are a lot of them in this game!
__________________
-Lisa, husband Ken age 60 dx SAA 7/04, dx hypo MDS 1/06 w/finding of trisomy 8; 2 ATGs, partial remission, still using cyclosporine |
|
#19
|
|||
|
|||
|
Greg and Lisa,
Thanks for the additional information! Greg, I appreciate the link to Dr. Sekeres webinar and I am signed up for it. Lisa, since I am new to the disease and the information, I am glad to hear that I am not the only one feeling the Catch -22 pinch. I will look over some of the other graphs and data that you spoke about. Thanks for all the great information! Janice
__________________
Female, age 52 - Diagnosed May, 2011 Hypoplastic MDS. Cytogenetics showing 2 abnormalities on chromosome 15. Blasts<5%, IPSS of 1. All blood counts low, but no treatment; watch and wait. Registered for MUD; on Feb. 23/12 two donor matches found but returned since not needed yet! |
|
#20
|
|||
|
|||
|
to be or not to be
Dear Janice, Lisa and Greg,
by chance I've come across your discussion, which caused anxiety and grief in me, since I lost a dear MDS-fellow-patient yesterday. My age, 10/10 transplant of her brother, good post-transplant development, then after six months of moderate shape one infection followed the other plus a severe liver GvhD... I am in a little leukemia-forum, which I present with three friends of mine. The members (only about 40, open for newcomers) meet once a year to spend a weekend together. So after the years, we have known each other personally and there are little regional meetings in between. When we meet, we definitely have fun, we eat and drink, have sight-seeing or just walk around a bit. But unfortunately we always have to say good-bye to several friends, who do not make it throughout the year. In 2010 we lost seven of us, this year we've lost two... Those who are "off the dangerous zone" had their transplants rather in their thirties or fourties... In fact there is only one ex-MDS-lady, who is rather well off. BUT in my patient support group there are three transplanted guys (45, 50 and 69 !) who are feeling fine after having been transplanted six months before. I hold them up as my models. NONE of them had a choice. SCT was the last option for all of them. I still have the choice, confirmed by my first, second and even third opinion. I repeatedly went on the nerves of my docs in three different mds-centres. All of them nodded their head. Even when my tx-frequency will increase (now I am due every 16 days...), NO recommendation for a SCT!!! They have been telling me that for 6 years now. I was informed, that there would be three cases which would alter my situation immediately and would lead to a SCT-decision. - a steady decline of white counts and platelets ( I am between 3,0-4,0 wbc and 250 000 plts) - an increase of blasts over 5% (I don't have any yet) - an additional chromosomical aberration (I have my trisomy 8, between 50 and 60 % also for six yrs now) Each of these changes would mean a severe progression of the disease. And then SCT will be my last option. Never before. I am very thankful that your discussion was so realistic, though hard to bear. Well, yes, SCT as a cure? I know all the statistics (of course I try to ignore them). There is only a few of us who will be lucky. Recently one doc said to me: "If I transplant you tomorrow, you might be dead within two months. If I don't do it, you will be alive much longer than that. Taking this into consideration, I never would recommend you for a SCT at the time being "? I know, I did not tell you "new things". But your posts have confirmed me again that watch&wait CAN be the best for some of us. It is the best for me. Thank you for reading and sharing. Solidary greetings, Bergit
__________________
female, 54, MDS-RCMD, trisomy 8, dx 2006, response to EPO and therafter VPA only for a couple of months, transfusion-dependent twice a month, watch&wait for SCT somewhen in the future with my brother as a donor 
|
|
#21
|
|||
|
|||
|
Hi Bergit,
I appreciate your response, and some of your findings from your group of friends in relation to SCT. You bring up an interesting fact, which was part of my original question and further discussion with Greg. That deals with the issue of age and fitness at the time of SCT. If we wait until we are sicker and older for the transplant, are we reducing the odds of a successful outcome? At the same time, if we do the transplant earlier, and it is not successful at some point in the process, are we shortening our lives when we could have just opted for various treatments. The first specialist that diagnosed me suggested the BMT/SCT realitivily soon (once there was a need for treatments), while the second specialist from an MDS center of excellence suggested treatments, buying time with the chance of perhaps new drugs becoming available and then the BMT may not be even necessary, but if it is, then it would be the last step. Of course during this time we age and become less prepared for the transplant. It is a difficult and individualized journey. I am sorry to hear about the loss of your friend. Thanks though for adding to our discussion. Since I have been newly diagnosed, this forum has been very educational and I appreciate the sharing of information and experiences! Janice
__________________
Female, age 52 - Diagnosed May, 2011 Hypoplastic MDS. Cytogenetics showing 2 abnormalities on chromosome 15. Blasts<5%, IPSS of 1. All blood counts low, but no treatment; watch and wait. Registered for MUD; on Feb. 23/12 two donor matches found but returned since not needed yet! |
|
#22
|
|||
|
|||
|
Quote:
I, too, am sorry to hear about your friend. But it's great to hear that you have such a neat support group. Your list of reasons for transplant hews very close to the rationale outlined by Dr. Matt Kalaycio of the Cleveland Clinic in the presentation that Lisa V and I have recommended. He says the Cleveland Clinic never transplants low-risk MDS patients, because, even though the success rate is highest with that group, that group has other options. Reasons they proceed to transplant: High IPSS Score High Probability of conversion to AML Intolerable transfusion requirement Severe Neutropenia. That's pretty similar to the criteria your doctors use. Take care! Greg
__________________
Greg, 59, dx MDS RCMD Int-1 03/10, 8+ & Dup1(q21q31). NIH Campath 11/2010. Non-responder. Tiny telomeres. TERT mutation. Danazol at NIH 12/11. TX independent 7/12. Pancreatitis 4/15. 15% blasts 4/16. DX RAEB-2. Beginning Vidaza to prep for MUD STC. Check out my blog at www.greghankins.com |
|
#23
|
|||
|
|||
|
Wow!
Wow! I am so happy that I found this discussion. All the good questions and eloquent discussions are exactly what I need right now. I am a 57 Yr. old female, recent Dx of hypoplastic MDS. My BMB showed no cytogenic abnormalities or blasts, but hypocellular marrow (10%). My doc thinks that I have a case of my immune system attacking my marrow, so maybe ATG/cyclosporine in the future as the best course of action (my counts are slowly declining -- now at WBC 3.8, RBC 2.27, Hct 25.4, Hgb 9.1, Plts 29). I have been grappling with exactly the issues that have been brought up in this discussion. I'm on watch and wait, but my shortness of breath has become quite severe. I have always been very healthy and athletic, doing many aerobic activities -- running, biking, swimming, cross-country skiing, etc. Now I'm to the point where I'm avoiding hills and stairs -- quite a change for me. So...my doc is recommending transfusion or growth factors (Epogen or Procrit) to help with my Hgb and Hct; he's leaving the choice up to me - yikes! IF my counts keep declining, he would then go to IST, and lastly to BMT. I am drug averse, so right now I'm grappling with whether or not to even try transfusions or growth factors. I would love to get my breath back, but, after watch and wait, I feel like this is jumping into the void with both feet, a void from which there is no escape. I guess I still have some disbelief that my disease is not going to get better on its own... I keep clinging to the fact that I have no cell or chromosomal abnormalities, and no blasts, but then there is the fact that my counts ARE declining, slowly but surely. Thanks for reading, and thanks to all, especially Greg, for the helpful links!
marmab |
|
#24
|
|||
|
|||
|
Hey Marmab!
I'm not doc, just a (I hope) well-informed patient who's done a lot of reading, so take what I'm about to say with a big grain of salt. I'm sorry to hear about your shortness of breath, particularly since you've been so active in the past. Everyone seems to be different in terms of what HgB level gives them trouble. 9.1 works fine for me, but my Hgb fell very gradually over a period of years (I think), and that may have given my body a chance to adjust. The ATG/cyclosporine recommendation makes sense, given that hypocellular marrow and younger age (isn't it nice to be part of a community where 50-something is "young!") are indicators that immunosuppressive therapy [IST] may be useful. If you decide to go that route, I'd encourage you to read this post, and either this thread or my blog, and check out the Campath trial at the National Institutes of Health. While it evidently hasn't worked for me, it has for others, and Campath, though still in trial stage, has some advantages over ATG/cyclosporine for MDS. It knocks down the T-cells more completely and for a longer period of time than ATG. So most folks who respond don't need the cyclosporine follow-up. It you cruise around marrowforums and read about cyclosporine, I think you'll find that it's a tricky drug to get right, with significant side effects. You may not have been HLA-typed at this point, because transplant would be way off in the future for you, but, if you have, and you are HLA-DR15 positive, you will definitely want to think long and hard about IST & Campath. That's an important market for likely success with the therapy. If your doc is recommending growth factors, your natural EPO level must be under 500, because they generally aren't prescribed for folks with higher levels. They actually work best, as I understand it, for patients with EPO under 100. RBC transfusions aren't bad. It takes the better part of a day in the treatment center, and, if you can stretch your interval out to six or eight weeks, the HgB bump can definitely get you more energy (and breath) for a minimal investment of time. Not all the fatigue from MDS is simply HgB, but that's definitely part of it. Have you consulted with a MDS expert? I don't know where in Mass you are, but Dr. David Steensma at Dana-Farber and Harvard is one of the noted experts in the field. Take Care! Greg
__________________
Greg, 59, dx MDS RCMD Int-1 03/10, 8+ & Dup1(q21q31). NIH Campath 11/2010. Non-responder. Tiny telomeres. TERT mutation. Danazol at NIH 12/11. TX independent 7/12. Pancreatitis 4/15. 15% blasts 4/16. DX RAEB-2. Beginning Vidaza to prep for MUD STC. Check out my blog at www.greghankins.com |
|
#25
|
|||
|
|||
|
I am 58 years old, also with chromosomal abnormality on 15 and hypo cellular bone marrow of 15%. Diagnosed SAA in UK September 2010, had ATG November 2010 and still receiving blood transfusions and cyclosporin. ATG did not work, but have remained relatively stable although transfusion dependent. Retired from work as teacher cos ANC less than 0.5 and kids really good at passing on infections! Asked about BMT cos have four siblings not tested as yet but got told don't cos am stable, and the risks are in excess of 30% mortality in first year and rising to nearly 50% after two years of BMT. This was Kings in London which is UK's centre of excellence giving this advice. There are days when I want all the crap to be over and I think BMT would sort it one way or the other, and other days when I feel the docs might have bothered at least to check my siblings. In general medicine progresses all the time and not going for BMT straightaway as your first course of treatment would not statistically affect your overall chances says my Statistics daughter. Suspect she may be biased! Wish you well, hope your disease goes into remission on its own and that you are spared these horrid choices. Either way there is always plenty of support on this site especially when you are at your lowest. I should know!
|
 |
| Thread Tools | Search this Thread |
|
|
 Similar Threads
Similar Threads
|
||||
| Thread | Thread Starter | Forum | Replies | Last Post |
| Acute Gvhd My Mom's Story | tamara669 | Tell Your Story | 26 | Sun Feb 7, 2016 02:08 AM |
| Double transplant - BMT and kidney (yes I might very well be crazy) | Ninanna | Tell Your Story | 7 | Tue Sep 9, 2014 08:24 AM |
| Questions to ASK at BMT Consult | NLJabbari | Transplants | 4 | Tue Oct 29, 2013 10:51 PM |
| BMT or NO BMT | shelby | Transplants | 5 | Mon May 6, 2013 12:45 PM |
| Update on BMT of 14th Feb 2007 | Nina van Nunen | Transplants | 4 | Mon May 28, 2007 04:59 PM |